DIAGNOSIS & DSM-5
Autism Symptom Disorder (ASD) is defined in the Diagnostic and Statistical Manual of Mental Disorders – Fifth Edition (DSM-5). The DSM-5, published in 2013 by the American Psychiatric Association (APA) is the principal authority used in the United States to specify the classification and classification codes of mental disorders.
< My Thoughts > “…used in the United States to specify…”, “…educational, social, and medical services…”
In the United States, data from geographical areas is used to evaluate trends over time. Thus, identifying and planning for future educational, social, and medical services. Hopefully, if the data shows an increase in autism diagnoses, then new community healthcare providers and educational settings will be provided, allowing more services for those individuals with autism.
Such data may also influence that when a child is from a ‘marginalized’ area, they will likely be considered ‘disadvantaged’, and the reason for their developmental delay. This may or may not be factual, but it should be helpful if parents are aware of this possible mindset when receiving or questioning a diagnosis.
Myers, et al. (2018) inform us that increases in the numbers of new ASD case identification is used in geographical areas, as needed for identifying and planning of educational, social, and medical services which are expected to be needed. They also evaluate trends over time, according to total special education and developmental services conducted.
Note: The DSM-5 Revised Edition (2013) replaced the previous edition, the DSM-4.
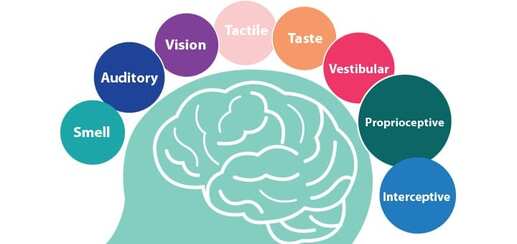
The DSM-5 Revised Edition (2013) has a new focus on ‘Sensory Behavior’ as a possible exhibition of how the autistic brain perceives the world. The new DSM-5 now emphases the ‘severity level’ of autistic behaviors. Indicated as well, are the specific categories for the diagnosed impairment (e.g., social communication and/or repetitive patterns of behavior). For example, a ‘DSM-5 severity level’ states ‘level of needs for support’.
• Level 1 – requiring support
• Level 2 – requiring substantial support
• Level 3 – requiring very substantial support
A child/adult may be diagnosed with ‘intense support’ for deficits in social communication; but only designated as needing ‘moderate support’ for restrictive repetitive behaviors.
SENSORY PROCESSING ISSUES –
- I can be sensitive to loud noises
- I don’t like to brush, wash, or cut my hair
- I like to smell people & objects, sometimes
- I don’t like tags on my clothes
- I don’t like to wear clothes
- I enjoy being squeezed, I like pressure
- I don’t want my hands dirty
- I have poor fine motor skills
- I get overstimulated & meltdown
- I get fearful & anxious sometimes
- I overreact to minor scrapes & cuts
- I cling to adults I trust
- I sometimes walk on my toes
- I have poor body awareness
- I crave fast spinning
- I lose my balance
- I like wearing the same clothes
- Sometimes, I don’t like to be touched
- I have poor gross motor skills
- I can be clumsy & fall over things sometimes
- I am a picky eater
- Some smells really bother me
- I don’t like bright lights
- I don’t like to brush my teeth
These are ‘sensory’ reactions, NEVER thoughtful nor planned responses. Also, they are very complex issues. Any or all ‘sensory’ reactions can cause these undesirable behaviors. Keep in mind that sensory excitement can trigger ‘stimming’ like hand-flapping, head-banging, hair pulling, scratching or biting. This seems to break the sensory processing circuit, bringing relief.
< My Thoughts > “…bringing relief.”
Sensory Processing Integration Therapy, which often looks like, and may be called – ‘Play Therapy’, is designed to help by desensitizing defensive and avoidance behavior.
Note: See more in Luker, S. (2024) UNIT 4 Chapter 3 – Sensory Integration.
Elwin, et al. (2016) talk about interesting remarks from participants in a study about sensory experiences which they followed. Here are some of those remarks –
- I often feel great discomfort when other people touch me.
- I feel no pain at times when other people think I should.
- When I look at certain patterns or colors or hear certain sounds or tones, I find them extremely fascinating.
- In everyday situations, I feel clumsy because I drop things, and sometimes I spill a lot.
- I can sit for hours on end looking at speckled bits of quartz inside stones.
- I have problems with daily routines and sleep.
< My Thoughts > “…looking at speckled bits of quartz …”
Take our Sonny into a jewelry store and he can be mesmerized for hours. Twinkling jewels, shiny rings and trinkets, plus the lighted cases and the soft music. He could stay there gazing for hours.
If Gardner (2008) gives her son Dale so much as a single pea or slice of carrot, he would protest by vomiting at will.
Cariello, C. (2015). 19% Much of Jack’s issues, it turns out, are related to sensory integration and his own internal regulation. …he struggles with regulation, cognitive flexibility, working memory and processing, and auditory and visual complexity.
< My Thoughts > “…his own internal regulation. …he struggles…”
This is another slippery slope with our Sonny. If he doesn’t intuit that he wants something or that he’s on sensory overload… the he just goes into his ‘flight or fight’ response. He overrides his ADHD medication and starts buzzing like a bee… stinging whatever or whomever crosses his path.
Living life with a lot of sensory issues, with the added problem of not being accepted can keep everyone from understanding how hurtful life can become. Somewhere, someone must be there for this person.
Potvin, J. E. (2013) 28% We asked our pediatrician what was wrong with Andrea. Why did she have all these odd quirks? Our doctor sent us to a specialist. After two minutes, he told us that Andrea also had autism. She displayed different signs than Sarah. Andrea did not flap like an eagle, but she did take her toys, dance around the room and make the same noises over and over.
< My Thoughts > “Why did she have all these odd quirks?”
The professional literature reflects that ‘odd quirks’ seem to be some sort of response the environment. The child or adult may have sensory issues, may be feeling anxious or excited, or having an obsessive compulsive moment. Somehow, the brain is telling the body to perform these ‘odd quirks’.
Kedar (2012) keeps us informed by saying, “Internal and external distractions – I can’t stop my senses. No one can. But mine overwhelm me. I hear my dog bark like a gunshot. My ears ring and I lose focus on my task.” Imagine living in a body that paces or flaps hands or twirls ribbons when your mind wants it to be still or, freezes when your mind pleads with it to react. At times your body charges forward impulsively, snatching things, or dashing you into the street.
< My Thoughts > “I can’t stop my senses.”
What this looks like at home, in the community, and at school is the child will cover his or her ears and may also stim excitedly. Sometimes the stimming is a delayed reaction, but it is still tied to being startled or overwhelmed by a noise or sound.
What is the most concerning or destructive thing that is going on right now in your child’s world?
Document concerning behaviors such as – ‘tantrumming’, and ‘I want it and I want it now’ behaviors, and ‘sensory meltdowns’. Note, that meltdowns are NOT usually a ‘thought-out’ behavior but a likely ‘sensory’ reaction. While these behaviors are high on the list of parental concerns, recent studies show the following things also worry parents.
Morin, A. (2018) tells us that… “The causes of tantrums and sensory meltdowns are different. Tantrums usually have a purpose. Kids are looking for a certain response. Sensory meltdowns are a reaction to something ‘sensory’ that is usually beyond a child’s control.”
Morin suggests that when responding to a tantrum try acknowledging that you know what your child wants, without giving in. Calmly tell them the reason that their needs (wants) can’t be met. Or, then tell them when they will be met. When responding to a sensory meltdown, help your child find a safe, quiet place away from the ‘sensory’ distress, where they can deescalate.
< My Thoughts > “…responding to a sensory meltdown…”
What to do while you wait for help, investigate, and prioritize concerns.
Parents often must wait days, weeks, and even months for assessments or doctor appointments. During this stressful time, it's good to feel that you are actively helping your child. This can become an important time of clarifying what bothers you the most about your child's behavior, development, or other concerns. Try to determine what may have ‘caused’ the concerning behavior. Granted, this may have only been a ‘trigger’ from the child’s perspective. Some behaviors remain a mystery, even to a trained observer. Video tape what you are seeing and how your child acts throughout the day/night. 'Seeing is believing' for someone new to your child.
References:
Cariello, C. (2015). What Color is Monday? How Autism Changed One Family for the Better; eBook Edition.
Elwin, M., et al. (2016). "Sensory clusters of adults with and without autism spectrum conditions." Journal of autism and developmental disorders 47 (2017): 579-589.
Gardner, N. (2008). A Friend Like Henry: The Remarkable True Story of An Autistic Boy & the Dog That Unlocked His World; eBook Edition.
Kedar, I. (2012). Ido in Autismland: Climbing Out of Autism; eBook Edition.
Luker, S. (2024); Know Autism, Know Your Child with < My Thoughts > by Sara Luker; Retrieved online from – www.sarasautismsite.com
Morin, A. (2018). The Difference Between Tantrums and Meltdowns; Retrieved online from – https://www.understood.org/en/learning-attention-issues/child-learning-disabilities/sensory-processing-issues/the-difference-between-tantrums-and-sensory-meltdowns
Myers, S., et al. (2018). Autism Spectrum Disorder: Incidence and Time Trends Over Two Decades in a Population-Based Birth Cohort; Journal of Autism & Developmental Disorders; V49, p1455-1474.
Potvin, J. E. (2013). Autism Triplet Twist: Survival Stories of Parents, Triplets and Autism; eBook Edition.
Note: DISCLAIMER – Autism ‘intervention’, as with the phrase ‘Early Detection / Early Intervention’, may simply mean to attempt an ‘action’, or attempt to ‘change a course’ or ‘trajectory’ of the person’s autism. Any expectation for a successful ‘change’ must have the cooperation of the participant, the parent, and/or the assigned therapist. Words such as, ‘intervention’, ‘treatment’, ‘therapy’, ‘service’, or ‘program’ imply ‘cure’, or ‘long-term’ positive effect. That is NOT my intention here, and all information is presented without intent or suggestion of status or effectiveness.
End of DAY FIFTEEN. Note: Excerpts from the books – (13% indicates location in the Kindle version of the eBook, instead of page numbers).
Sharing of my website and BLOG Comments welcomed. Thank-you to those of you who have sent comments... much appreciated!
Regards,
Sara Luker




 RSS Feed
RSS Feed