KNOW AUTISM, KNOW YOUR CHILD; with < My Thoughts > by Sara Luker
UNIT 1 – Chapter #1 How Will I Know It's Autism?
INTRODUCTION ~
CHAPTER 1 – Checklists
CHAPTER 2 – Red Flags
CHAPTER 3 – Centers for Disease Control & Prevention (CDC)
PART 1. Developmental Screening
UNIT 1 – REFERENCES
UNIT 1 – APPENDIX A Informal Checklist with < My Thoughts > by Sara Luker
How Will I Know It's Autism?
Is it autism? What you can do while you are waiting for the world of doctor’s appointments, consultations, and program possibilities to open up to you…
< My Thoughts > "While You Wait... Investigate"
Parents often must wait days, weeks, and even months for assessments or doctor appointments. During this stressful time, it's good to feel that you are actively helping your child. This can become an important time of clarifying what bothers you the most about your child's behavior, development, or other concerns. Video tape what you are seeing. Show your concerns about how your child acts throughout the day/night. 'Seeing is believing' for someone new to your child.
Prioritize your child's 'needs' and your 'wants'. Try new things... like teaching your child age appropriate 'developmental skills' that are non-invasive. See what works and what doesn't. Eventually, you will have to choose from available programs, therapies, and services that will be offered. Some are quite expensive, so understand your child well enough to figure out what will probably work and what absolutely won't. You can only know this by trying some things on your own.
Try to know which are possible autism signs... and what is just your child's way of understanding their world. Red Flag signs may be very 'subtle' when a child has mild developmental delays. The ‘nots’, ‘doesn’ts’, ‘lack ofs’, and ‘inflexibles’ may mean that the child rarely gets happily excited over the little things, or may react unhappily instead. The child has little or no ‘back and forth’ communication responses, easy reciprocal smiles, giggles or joyful pleasure when with others.
PLEASE READ DISCLAIMER
UNIT #1; Chapter 1~ HOW WILL I KNOW IF IT IS AUTISM? A parent asked me where to find a list of 'red flags' & a 'checklist'. Here is a start ~
UNIT 1 – Chapter #1 How Will I Know It's Autism?
INTRODUCTION ~
CHAPTER 1 – Checklists
CHAPTER 2 – Red Flags
CHAPTER 3 – Centers for Disease Control & Prevention (CDC)
PART 1. Developmental Screening
UNIT 1 – REFERENCES
UNIT 1 – APPENDIX A Informal Checklist with < My Thoughts > by Sara Luker
How Will I Know It's Autism?
Is it autism? What you can do while you are waiting for the world of doctor’s appointments, consultations, and program possibilities to open up to you…
< My Thoughts > "While You Wait... Investigate"
Parents often must wait days, weeks, and even months for assessments or doctor appointments. During this stressful time, it's good to feel that you are actively helping your child. This can become an important time of clarifying what bothers you the most about your child's behavior, development, or other concerns. Video tape what you are seeing. Show your concerns about how your child acts throughout the day/night. 'Seeing is believing' for someone new to your child.
Prioritize your child's 'needs' and your 'wants'. Try new things... like teaching your child age appropriate 'developmental skills' that are non-invasive. See what works and what doesn't. Eventually, you will have to choose from available programs, therapies, and services that will be offered. Some are quite expensive, so understand your child well enough to figure out what will probably work and what absolutely won't. You can only know this by trying some things on your own.
Try to know which are possible autism signs... and what is just your child's way of understanding their world. Red Flag signs may be very 'subtle' when a child has mild developmental delays. The ‘nots’, ‘doesn’ts’, ‘lack ofs’, and ‘inflexibles’ may mean that the child rarely gets happily excited over the little things, or may react unhappily instead. The child has little or no ‘back and forth’ communication responses, easy reciprocal smiles, giggles or joyful pleasure when with others.
PLEASE READ DISCLAIMER
UNIT #1; Chapter 1~ HOW WILL I KNOW IF IT IS AUTISM? A parent asked me where to find a list of 'red flags' & a 'checklist'. Here is a start ~
PLEASE READ DISCLAIMER –
UNIT 1 – How Will I Know If It Is Autism?
INTRODUCTION
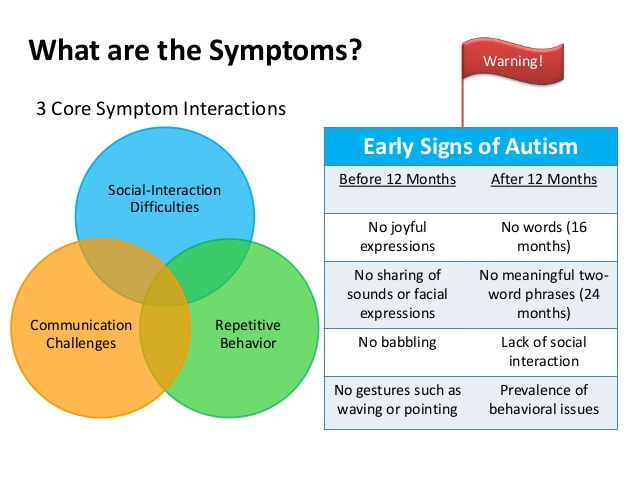
One of the ways parents may begin to know whether or not a child has autism, could be by comparing your child’s behavior with guidelines from the Centers for Disease Control & Prevention (CDC).
< My Thoughts > “…guidelines from the CDC.”
Although informal, the CDC guidelines are a way to begin knowing your child. Concerns about you child’s behavior can then be brought to the attention of your doctor. Keep notes about your observations and concerns. It may be helpful to phone videotape your child in action.
Clinicians throughout the world currently use the Diagnostic & Statistical Manual of Mental Disorders, Fifth Edition, DSM-5 (2013); published by American Psychiatric Association (APA), Washington, DC. This gives the definition of ‘autism’ as a developmental disorder which affects communication and behavior; with symptoms generally appearing in the first two years of life.
For parents, the DSM-5 diagnostic emphasis tends to be on the ‘sensory’ issues, which may add to identifying a child’s unusual, erratic, or harmful behavior. For clinicians, the DSM-5 diagnostic emphasis tends to be on ‘CODING’ references, necessary to medical offices and insurance companies in identifying the child’s diagnosis.
The DSM-5 clarifies the ways that a person’s symptoms may be identified, rated, and considered for services and insurance coverage. In the past, a person’s original diagnosis, from the previous DSM-4, and a more recent diagnosis from the DSM-5, might differ. This difference may require new investigation, or cause parents, clinicians, and insurance providers new concerns.
< My Thoughts > “…difference may require new investigation…”
Autism is classified, described and recognized as it appears in the Diagnostic & Statistical Manual of Mental Disorders; therefore, it is considered a ‘disorder’, instead of a ‘disability’. But where certain government and insurance agencies are concerned, an ‘autism disorder’ qualifies as a ‘disability’ for purposes of provider recognition.
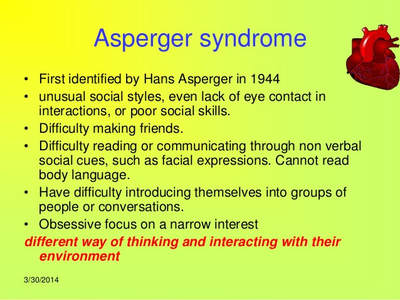
Autism first appeared in the previous DSM-4 as a subset of childhood schizophrenia. Now, in the current DSM-5, autism has an ‘umbrella’ classification as a spectrum of conditions and ‘developmental disorders’. Also, a clarification of impairments varying in their ‘severity levels’; mainly to include ‘social-emotional reciprocity’, ‘verbal and non-verbal communication’, and/or ‘restricted, repetitive patterns of behavior’.
Mayo Clinic Staff Writer (2020) makes it clear that there is no ‘cure’ for autism; but, that intensive early ‘treatment’ can make a big difference in the lives of ‘many’ children. In the writer’s ‘Overview’, further clarification states that Autism Spectrum Disorder, commonly known as ‘autism’, or ASD, begins in childhood; creating lifelong problems with functioning in society, at school, and in a work environment.
Signs of autism are usually seen by the time the child is 2 years old. A small number of children develop normally, then between 18 and 24 months of age, they change. These children may lose the language skills that they have already acquired, and may become withdrawn or even aggressive. Others on the spectrum may show normal to high intelligence, yet begin to have difficulty showing that intelligence when communicating, or in applying what they know to everyday situations.
Autism is unique because of the severity level of the symptoms, the mixture of symptoms, limited interests, and excessive unwanted behaviors. While autism affects children of all races and nationalities, some children may have the added risk factors of –
- Being born a boy. Boys have been shown to be 4 times more likely to have autism than girls, the data shows.
- Being born into a family with a history of relatives having autism is not an uncommon fact.
- Being born to aging parents seems to have an influence, although this has yet to be proven.
- Being born extremely prematurely; birth before 26 weeks, can be considered a greater risk.
- Being born with other disorders present; such as – Fragile X Syndrome (causes intellectual problems), Rett Syndrome (slow head growth, intellectual disability, and loss of purposeful hand use), Tuberous Sclerosis (benign tumors on the brain).
< My Thoughts > “…added risk factors…”
Other concerns which may complicate or delay diagnosis are added ‘risk factors’ such as –
- When girls are not diagnosed until as an adolescent, their unusual behaviors or predilections become more pronounced. Girls who are ‘high-functioning’ may also be ‘hard-wired’ to cope, problem solve, and will strive not to appear ‘different’.
- When a family’s genetic history is hard to track. Uncle Bob always did act a little ‘different’. Was it autism?
- When the child’s autism is associated with ‘parent’s age’. Someone actually said to me, concerning Sonny’s autism, “That’s what you get for having a kid ‘at your age’.”
- When discussions focus on ‘at-risk births’; or, if it is a disadvantage not to have a vaginal birth.
- When as the number of children diagnosed with autism increases, the reason for the increase seems to draw intense or somewhat confusing discussions. Was the child ‘born with’ autism? Does the child have ‘another’ disorder, with ‘autistic-like’ symptoms? Or, has the new awareness about autism led to a greater number of children being assessed and/or referred by clinicians.
All of these concerns raise additional questions. Although, little ‘real evidence’ exists, many more ‘autism-causing’ theories are out there. Also, to be considered may be whether there has been parental drug use before, or at the time of, conception. Did the mother have a viral infection during pregnancy? Has the exposure to all kinds of unhealthy environments during the child’s developmental period, been the cause? Or, have the numerous ‘developmental delays’ been due to ‘sensory sensitivities’; which when untreated, distract from learning and cause delays. To answer these questions, and your own, you will start to become a ‘trained observer’.
Christensen, et al. (2019) tell us that Autism Spectrum Disorder (ASD) is estimated to affect up to 3% of children in the United States; over a 3-year period (2010, 2012, & 2014). Early Age Identification, under 3 years of age, for ASD is considered necessary, so that evidence-based interventions can begin as early as possible. Within the participants in this group, they found ASD prevalence to be higher among boys than girls; and, a higher prevalence among non-Hispanic and White children; than among Hispanic or Black children.
< My Thoughts > “ASD prevalence was higher among boys than girls…”
Any data is only as good as the population from which it is collected. Many ‘at-risk’ children in ‘marginal’ populations may not be identified as being ‘ASD’ until they reach school age; when the social and cognitive demands exceed their current abilities. Also, parents may hardly notice troubling deficits in social reciprocity; nor do they always recognize ‘sensory stress’ behaviors in their children. They just notice that ‘something’ seems to be wrong. Parents may believe that it’s their parenting, before they consider that their child is struggling with a disorder.
As a child, I had a beloved book about an Indian boy named, “If he isn’t here, he’s some other place.” Nicknamed, “If he isn’t here,” this Indian boy was busy in his own world, and would seldom answer when his mother called for him. Throughout the book she explained his frequent absence in awareness by saying – “If he isn’t here, he’s some ‘other’ place.” Little did I know then, that I too would have a boy who was forever ‘absent’ when I called his name. A child who forever seemed to be some ‘other’ place. A child with Autism.
Our Sonny is nonverbal because in addition to ‘profound’ autism, we were told that the frontal lobe of his brain has never fully developed. He’s handsome, sweet and loveable, except when he isn’t. He can laugh, doesn’t cry, but can yell, making a variety of happy and mad sounds or grunts. He communicates with a few modified ‘baby sign-language’ signs, and the use of a simple assistive technology push-button device. When he does suddenly hear us or see us, he usually has a ‘startled expression’ which asks – “Who are you and where did you come from?”
Staff Writer (2013) finds that the word ‘Autism’ has as its roots the Greek words ‘autos’ and ‘ismos’; which means ‘self’ and ‘state of being’, respectively. Much of the time, an autistic child appears to exist outside the existence of other people in his or her surroundings.
Fallows (2014) finds Autism Spectrum Disorder (ASD), as clinically diagnosed, according to the current APA Diagnostic & Statistical Manual of Mental Disorders (DSM), to be a very complex disorder. This is due to the varying ages of onset, as well as the varying degrees of marked impairment. Autism also varies greatly in the range of severity, of each individual’s impairment. Each person with autism will present with their own version or complex pattern of autism. With subtle to severe changes occurring within each developmental stage, age, or trajectory throughout a person’s lifespan.
Mandy (2013) mentions that the newest edition of the Diagnostic and Statistical Manual of Mental Disorders, the DSM-5, overtly acknowledges that females with autism may have features that differ from those of males with the disorder. One of the most striking features of autism is its gender ratio. Males are four times more likely than females to receive an autism diagnosis, and at the high-functioning end of the autism spectrum there are as many as nine males for every female.
< My Thoughts > “…nine males for every female.”
One of the reasons for this early data, may be that the early diagnostic focus was on boys. Dr. Mandy has been one of the pioneers in championing girls and women on the autism spectrum. He has brought to the world’s attention that just because females with high-functioning autism may learn to be concealed within their clever camouflage, doesn’t mean that we can fail to recognize their needs.
Mandy points out that the architects of the DSM-5 have laid down a challenge to researchers. The challenge is to provide an account of the female phenotype, so that clinicians can learn to better identify, and help, females on the autism spectrum. They question why autism manifests more subtly in females, and is therefore misdiagnosed as an anxiety or personality disorder. Questioning too, whether repetitive behaviors in females with autism, present in more socially normative ways, And, whether females with the disorder have a greater capacity to hide, camouflage, or compensate for their difficulties.
Satel (2014) acknowledges that having a diagnosis using the Diagnostic & Statistical Manual of Mental Disorders (DSM) published by American Psychiatric Association (APA), can carry ‘unwarranted clout’. Diagnoses, even if imprecise, can command resources; can mean insurance coverage, access to special educational and behavioral services in schools, and eligibility for disability benefits.
< My Thoughts > “…unwarranted clout.”
The DSM-5 emphasis on ‘Sensory Issues’ will allow new referrals to clinicians, specialists, and therapists. In turn, an Occupational Therapist can then provide an assessment for Sensory Integration Therapy; or, recommend other services for that child. Helpful, because over time sensory stress issues can be recognized as the possible cause of severely disruptive behavior. Have your child ‘identified’ so services can begin as soon as possible. With early ‘intervention’ comes hope. Know also, that your child may have learning and/or behavior issues unrelated to ‘autism’. In other words, a child with Attention Deficit Hyperactivity Disorder, MAY or MAY NOT have autism. One does NOT automatically indicate the other.
Note: The DSM-5 is a diagnostic tool used mainly by clinicians in the United States and Canada; but it is also known and consulted by professionals around the world.
CDC Staff Writer (2020) for the Centers for Disease Control & Prevention (CDC) describes autism as a developmental disorder, which can cause significant social, behavioral, and communication challenges –
- Disrupting successful learning within school settings
- Preventing an ability to live independently
- Creating an inability to be successfully employed
- Causing social isolation or rejection
- Producing stress within families
- Allowing for victimization & bullying
A person with autism’s optimistic future outcome and adequate functioning calls for ‘early intervention’; in the areas of behavior, language, communication, and/or sensory domains. A variety of treatment options are necessary, so that they may be able to function adequately. Treatment is important because the CDC states that there is considered to be NO current ‘cure’ for autism.
CHAPTER 1 – CHECKLISTS
CHECKLISTS –
Image shows Centers for Disease Control & Prevention (CDC) Phone TrackerApp: Retrieved from – cdc.gov/MilestoneTracker
Whiffen (2009) shares concerns about her son – Finally home, I hurry to my computer. I place my fingers on the keyboard and type “AUTISM”. My pinky finger hangs over the Enter key, frozen. My fear has definition. I am afraid of what I might find.
That evening, I go to bed unable to sleep, I go back downstairs. I press the Enter key, I force myself to look at the “Autism Signs & Symptoms” checklist –
My eyes filled with tears as I looked at this description of my son on the computer.
I also find an online Time magazine article, “The Secrets of Autism” (2002) by Madeleine Nash. At the end of the article it says, “Paradoxically, the very thing that is so terrible about autistic disorders is that they affect the very young. But they suggest a reason for hope, since the neural connections of a child’s brain are established through experience, well-targeted mental exercises have the potential to make a difference.” What catches my attention is Nash says an ‘early diagnosis’ has become increasingly important. I discover that I don’t even ‘have’ months. Sifting through the masses of research could take years.
< My Thoughts > “…could take years…”
My thoughts, exactly. Sifting through the masses of research could take years. Thus, the critical need to share my researching, brought about my Website and Blog on www.sarasautismsite.com, and eventually this material.
Hearing the words “this child has autism,” parents, are often ‘stunned’. Then, in the face of so many more questions racing through their minds, the doctor says, “Just go on the autism websites and read everything you can about autism.” Yes, disturbingly this kind of professional advice is still given to too many of our families.
Next, my task became finding and reading as many current books, and peer-referenced journal articles and reviews on autism as I could. I wanted to get more answers for myself, for my son, and for others. Soon, my purpose became to reach out for those who find themselves desperately searching for answers about autism.
As an educator, and parent of an adult-child with autism, my hope became to provide other parents, family members, caregivers, teachers, clinicians, and academics with the information needed to understand what it means to know a child on the autism spectrum. And, sometimes its years before a person discovers that they too are on the spectrum.
Squaresky (2014) states that her son Greg became obsessed with Sesame Street. When he was a one-year-old, he did thirty-piece puzzles. The new baby next door couldn’t do anything except eat, cry, and play with a rattle; but not Greg. Clearly, he was brilliant.
He had some quirky behaviors that we explained away easily. His repetitive play confused us, as much as it entertained us. After all, how many children stayed at a task for hours?
I faithfully recorded each new word in his baby book and according to our pediatrician, the same doctor that my husband Jay had as a child, 18-month-old Greg was developing normally. I don’t know how Dr. Karp ever came to that conclusion, since Greg screamed through every appointment.
< My Thoughts > “…screamed through every appointment.”
Even today, a child screaming through every appointment may have people explaining it away; without thoughts of sensory issues, or thoughts of autism. Many neuro-typical children may scream through appointments, until they become old enough to understand the ‘what’ and ‘why’ of doctor’s offices. And, that doctors aren’t out to ‘hurt’ children.
But parents checking CHECKLISTS can be just a first step. The diagnosis has to come from the DSM-5 Checklist, i.e., ‘criteria’, completed by a qualified professional. Therefore, your pediatrician, or clinician must stay with you long enough to make a decision about a diagnosis. You may have to ask your physician if s/he feels qualified to make that decision, or if they would like to refer you to a specialist.
Always, do your homework and ‘identify but verify’. Almost everyone you find yourself dealing with is in ‘business’; expecting to receive the monies necessary to continue. Remember too, that there is a difference between ‘short term’ and ‘long term’ programs. If you sign on to a long-term program, that could mean ‘years’ of a therapy that may or may not be working over the trajectory of your child’s autism symptoms.
Major, et al. (2013), brought to light the fact that there has been little focus on improving ASD education, during pediatric residency. This study evaluated the curriculum regarding autism, which was currently being taught to future doctors.
The 7 case-based Autism curriculum modules addressed were –
1. Early warning signs of Autism
2. Screening for Autism
3. Communicating concerns: Screening/diagnostic results
4. Making an Autism diagnosis
5. Early intervention & education
6. Treatments for Autism
7. Autism-specific anticipatory guidance
In their conclusion, the authors stated that most pediatric residents felt that autism training was important to their careers; but, that the current program of 7-case-based Autism modules were very brief and therefore inadequate. Finally, at the end of this training, they rated their overall competence in preparation for diagnosing Autism Spectrum Disorder (ASD) as poor.
< My Thoughts > “…they rated their overall competence as poor.”
After their training, the new pediatric residents rated their overall feelings of competency regarding training for diagnosing ASD, as inadequate. With that rating, the chances of parents receiving an ‘early intervention’ recommendation from those new pediatric residents would not be too hopeful.
Improving ASD education to future doctors, might include the fact that some parents may unknowingly, be hoping to see a doctor who ‘looks like them’; or, is at least from a background of cultural diversity.
Added to that, families who live in a marginalized community, or are an ‘ethnic other’ find their options of discovering ‘early intervention’ are few. Also, pediatricians who have been in practice for a number of years, may want to learn about the possible need to provide autism screening for their challenging patients, of all ages.
Gonzalez, et al. (2015) offered a study which was designed to show how children with disabilities improved over time, with ‘early intervention’ for all. Instead, they discovered that there was a huge disparity between the ‘white’ children being treated with early intervention, and the treatment of ‘ethnic others’ receiving early services.
Among the reasons they gave was the family’s lack of access to traditional medical services, and/or any health care providers. Another reason was that pediatricians were not always (or, were rarely) trained to become familiar with the early identification, and/or the autism referral practices available in their community. And, that there seemed to be a lack of health insurance recommended/accepted healthcare providers available; in spite of the Individuals with Disabilities Education Act (IDEA) Part C, stating that the families are to receive services, regardless of their ability to pay.
< My Thoughts > “…early identification…”
The pediatrician or clinician may only see the child during a cursory visit before having the series of immunization needed for school. ‘Well-check’ visits are not always encouraged or covered by insurance companies; nor are they done traditionally in certain populations. When parents are asked, “What did the doctor say during your child’s routine ‘Well-check’ visit?” Often, the answer is,” What is a Well-check’ visit?”
Some pediatricians Gonzalez reported, took the ‘wait & see’ approach to developmental delays recognized in early visits. Again, physicians didn’t know where to refer families next. Or, in the rare cases where doctors did identify children, families experienced long appointment delays; or, the parents did not want to follow-up with recommendations, for whatever reasons. Often times, the reason was because the healthcare providers available didn’t look like them. In other words, there was very little choice of clinicians with cultural or ethnic diversity.
REFERENCES: UNIT 1 – CHAPTER 1 CHECKLISTS
CDC (Centers for Disease Control & Prevention) Staff Writer (2020). Autism A Developmental Disability; Retrieved online from – https://www.cdc.gov/
Christensen, D., Maenner, M., et al. (2019). Prevalence & Characteristics of ASD Among Children Aged 4 Years – Early Autism & Developmental Disabilities Monitoring Network, Seven Sites, U.S, 2010, 2012, & 2014; Surveillance Summaries: US Dept. of Health & Human Services/Centers Control & Prevention; V68:2, p1-14.
DSM-4 (1994). American Psychiatric Association; Diagnostic & Statistical Manual of Mental Disorders (4th Edition); Washington, DC.
DSM-5 (2013). American Psychiatric Association; Diagnostic & Statistical Manual of Mental Disorders (5th Edition); Washington, DC.
Fallows, A. (2014). Can Autism Be Treated Successfully with Homoeopathic Medicine?; Journal of the Australian Traditional–Medicine Society; V20:2, p120-123.
Gonzalez, E., Summers, C., et al. (2015). Developmental Surveillance & Referral in a Traditionally Medically Underserved Border Community; Maternal Child Health, V19, p2323-2328.
Major, N., Peacock, G., et al. (2013). Autism Training in Pediatric Residency: Evaluation of a Case-Based Curriculum; Journal of Autism & Developmental Disorders; V43; p1171-1177.
Mandy, W. (2013). DSM-5 May Better Serve Girls with Autism; Retrieved online from – www.spectrumnews.org/
Mayo Clinic Staff Writer (2020). Autism Spectrum Disorder, Overview: Mayo Clinic Rochester, MN.; Retrieved online from – https://www.mayoclinic.org/
Nash, M. (2002). The Secrets of Autism; Time magazine article.
Satel, S. (2014). DSM-IV & DSM-V Differences: Ending the Confusion; Retrieved online from – Counselling Connection > Clinical Mental Health > DSM-IV and DSM-V Differences: Ending the Confusion.
Squaresky, M. (2014). A Spot on the Wall; eBook Edition.
Staff Writer (2013). Autism; Retrieved online from – http://www.autismepicenter.com/
Whiffen, L. (2009). A Child’s Journey Out of Autism: One Family’s Story of Living in Hope and Finding a Cure; eBook Edition.
UNIT 1 – CHAPTER 1 APPENDIX A – Parent Concerns Informal Checklist (Similar to CDC online checklist)
Child’s Name _________________________
Date of Birth ________ Parent’s Name______________
My Child
< Answer (Pick one) Yes, Some-times, or No >
Responds to name
Says 10 (or more) words
Learns new words, weekly
Repeats new words heard
Repeats a new or familiar word over & over, constantly
Says 50 (or more) words
Puts 2 words together, independently
Gets my attention with words
Rejects something by saying “No”
Asks questions by changing voice to indicate s/he is asking a question
Takes turns in a conversation (engages in a back-and-forth)
Asks for help with words
Says understandable 3-4 word sentences
Is easily understood by other family members
Is easily understood by familiar adults
Is easily understood by unfamiliar adults
Follows one-step directions
Follows two-step directions
Listens to story being read in short picture book
Names the pictures in the book (interaction with reader)
Answers “Yes” or “No” questions
Asks “Yes” or “No” questions
Asks “wh” questions (who, when, where, what, why, how)
Uses pronouns correctly (I, me, we… instead of using person’s name)
Knows some songs or nursery rhymes
Participates in pretend play (plays mommy/daddy, teacher, doctor)
Very active, always in motion (hyperactive)
Acts without fear of consequences (impulsive)
Points to objects s/he sees or wants
Unusual reaction to the way things sound, smell, feel, taste or look
Throws tantrums (goal oriented, wants something that’s been denied, needs audience to be watching, trying to get control of others)
Has meltdowns (doesn’t know what’s wrong, it may be ‘sensory’ or other ‘overload’ or s/he may be overwhelmed by what is happening, emotions seem out of control)
Lines up toys or other objects, obsessively, engages in self-stimulatory behavior
Plays with the same toys the same way every time
Needs to follow a routine or ritual (bedtime, eating, and/or getting dressed)
Flaps hands, rocks body, or spins self in circles (or watches spinning things for a long period of time). Add something odd that you are noticing? _________________________
Only eats certain foods
Has difficulty feeding oneself
Can use pincher fingers to pick-up food
Uses utensils to eat food
Seems clumsy or uncoordinated
Can play on age-appropriate playground equipment
Plays well with siblings & same-age children
Note: The above is 'Informal data' to share with clinicians. Video on cell phone is helpful, too.
CHAPTER 1 – RED FLAGS
Whiffen (2009) shares concerns about her son – Finally home, I hurry to my computer. I place my fingers on the keyboard and type “AUTISM”. My pinky finger hangs over the Enter key, frozen. My fear has definition. I am afraid of what I might find.
That evening, I go to bed unable to sleep, I go back downstairs. I press the Enter key, I force myself to look at the “Autism Signs & Symptoms” checklist –
- Inappropriate laughing and giggling. CHECK!
- No real fear of danger. CHECK!
- Apparent insensitivity to pain. CHECK!
- May NOT want cuddling or act cuddly. CHECK!
- Little or no eye contact. CHECK!
- Difficulty expressing needs. CHECK!
- NOT responsive to verbal cues. CHECK!
- Sustains odd play. CHECK! CHECK! CHECK!
- Inappropriate attachment to objects. CHECK!
- Insistence on sameness; resists change in routine. CHECK!
My eyes filled with tears as I looked at this description of my son on the computer.
I also find an online Time magazine article, “The Secrets of Autism” (2002) by Madeleine Nash. At the end of the article it says, “Paradoxically, the very thing that is so terrible about autistic disorders is that they affect the very young. But they suggest a reason for hope, since the neural connections of a child’s brain are established through experience, well-targeted mental exercises have the potential to make a difference.” What catches my attention is Nash says an ‘early diagnosis’ has become increasingly important. I discover that I don’t even ‘have’ months. Sifting through the masses of research could take years.
< My Thoughts > “…could take years…”
My thoughts, exactly. Sifting through the masses of research could take years. Thus, the critical need to share my researching, brought about my Website and Blog on www.sarasautismsite.com, and eventually this material.
Hearing the words “this child has autism,” parents, are often ‘stunned’. Then, in the face of so many more questions racing through their minds, the doctor says, “Just go on the autism websites and read everything you can about autism.” Yes, disturbingly this kind of professional advice is still given to too many of our families.
Next, my task became finding and reading as many current books, and peer-referenced journal articles and reviews on autism as I could. I wanted to get more answers for myself, for my son, and for others. Soon, my purpose became to reach out for those who find themselves desperately searching for answers about autism.
As an educator, and parent of an adult-child with autism, my hope became to provide other parents, family members, caregivers, teachers, clinicians, and academics with the information needed to understand what it means to know a child on the autism spectrum. And, sometimes its years before a person discovers that they too are on the spectrum.
Squaresky (2014) states that her son Greg became obsessed with Sesame Street. When he was a one-year-old, he did thirty-piece puzzles. The new baby next door couldn’t do anything except eat, cry, and play with a rattle; but not Greg. Clearly, he was brilliant.
He had some quirky behaviors that we explained away easily. His repetitive play confused us, as much as it entertained us. After all, how many children stayed at a task for hours?
I faithfully recorded each new word in his baby book and according to our pediatrician, the same doctor that my husband Jay had as a child, 18-month-old Greg was developing normally. I don’t know how Dr. Karp ever came to that conclusion, since Greg screamed through every appointment.
< My Thoughts > “…screamed through every appointment.”
Even today, a child screaming through every appointment may have people explaining it away; without thoughts of sensory issues, or thoughts of autism. Many neuro-typical children may scream through appointments, until they become old enough to understand the ‘what’ and ‘why’ of doctor’s offices. And, that doctors aren’t out to ‘hurt’ children.
But parents checking CHECKLISTS can be just a first step. The diagnosis has to come from the DSM-5 Checklist, i.e., ‘criteria’, completed by a qualified professional. Therefore, your pediatrician, or clinician must stay with you long enough to make a decision about a diagnosis. You may have to ask your physician if s/he feels qualified to make that decision, or if they would like to refer you to a specialist.
Always, do your homework and ‘identify but verify’. Almost everyone you find yourself dealing with is in ‘business’; expecting to receive the monies necessary to continue. Remember too, that there is a difference between ‘short term’ and ‘long term’ programs. If you sign on to a long-term program, that could mean ‘years’ of a therapy that may or may not be working over the trajectory of your child’s autism symptoms.
Major, et al. (2013), brought to light the fact that there has been little focus on improving ASD education, during pediatric residency. This study evaluated the curriculum regarding autism, which was currently being taught to future doctors.
The 7 case-based Autism curriculum modules addressed were –
1. Early warning signs of Autism
2. Screening for Autism
3. Communicating concerns: Screening/diagnostic results
4. Making an Autism diagnosis
5. Early intervention & education
6. Treatments for Autism
7. Autism-specific anticipatory guidance
In their conclusion, the authors stated that most pediatric residents felt that autism training was important to their careers; but, that the current program of 7-case-based Autism modules were very brief and therefore inadequate. Finally, at the end of this training, they rated their overall competence in preparation for diagnosing Autism Spectrum Disorder (ASD) as poor.
< My Thoughts > “…they rated their overall competence as poor.”
After their training, the new pediatric residents rated their overall feelings of competency regarding training for diagnosing ASD, as inadequate. With that rating, the chances of parents receiving an ‘early intervention’ recommendation from those new pediatric residents would not be too hopeful.
Improving ASD education to future doctors, might include the fact that some parents may unknowingly, be hoping to see a doctor who ‘looks like them’; or, is at least from a background of cultural diversity.
Added to that, families who live in a marginalized community, or are an ‘ethnic other’ find their options of discovering ‘early intervention’ are few. Also, pediatricians who have been in practice for a number of years, may want to learn about the possible need to provide autism screening for their challenging patients, of all ages.
Gonzalez, et al. (2015) offered a study which was designed to show how children with disabilities improved over time, with ‘early intervention’ for all. Instead, they discovered that there was a huge disparity between the ‘white’ children being treated with early intervention, and the treatment of ‘ethnic others’ receiving early services.
Among the reasons they gave was the family’s lack of access to traditional medical services, and/or any health care providers. Another reason was that pediatricians were not always (or, were rarely) trained to become familiar with the early identification, and/or the autism referral practices available in their community. And, that there seemed to be a lack of health insurance recommended/accepted healthcare providers available; in spite of the Individuals with Disabilities Education Act (IDEA) Part C, stating that the families are to receive services, regardless of their ability to pay.
< My Thoughts > “…early identification…”
The pediatrician or clinician may only see the child during a cursory visit before having the series of immunization needed for school. ‘Well-check’ visits are not always encouraged or covered by insurance companies; nor are they done traditionally in certain populations. When parents are asked, “What did the doctor say during your child’s routine ‘Well-check’ visit?” Often, the answer is,” What is a Well-check’ visit?”
Some pediatricians Gonzalez reported, took the ‘wait & see’ approach to developmental delays recognized in early visits. Again, physicians didn’t know where to refer families next. Or, in the rare cases where doctors did identify children, families experienced long appointment delays; or, the parents did not want to follow-up with recommendations, for whatever reasons. Often times, the reason was because the healthcare providers available didn’t look like them. In other words, there was very little choice of clinicians with cultural or ethnic diversity.
REFERENCES: UNIT 1 – CHAPTER 1 CHECKLISTS
CDC (Centers for Disease Control & Prevention) Staff Writer (2020). Autism A Developmental Disability; Retrieved online from – https://www.cdc.gov/
Christensen, D., Maenner, M., et al. (2019). Prevalence & Characteristics of ASD Among Children Aged 4 Years – Early Autism & Developmental Disabilities Monitoring Network, Seven Sites, U.S, 2010, 2012, & 2014; Surveillance Summaries: US Dept. of Health & Human Services/Centers Control & Prevention; V68:2, p1-14.
DSM-4 (1994). American Psychiatric Association; Diagnostic & Statistical Manual of Mental Disorders (4th Edition); Washington, DC.
DSM-5 (2013). American Psychiatric Association; Diagnostic & Statistical Manual of Mental Disorders (5th Edition); Washington, DC.
Fallows, A. (2014). Can Autism Be Treated Successfully with Homoeopathic Medicine?; Journal of the Australian Traditional–Medicine Society; V20:2, p120-123.
Gonzalez, E., Summers, C., et al. (2015). Developmental Surveillance & Referral in a Traditionally Medically Underserved Border Community; Maternal Child Health, V19, p2323-2328.
Major, N., Peacock, G., et al. (2013). Autism Training in Pediatric Residency: Evaluation of a Case-Based Curriculum; Journal of Autism & Developmental Disorders; V43; p1171-1177.
Mandy, W. (2013). DSM-5 May Better Serve Girls with Autism; Retrieved online from – www.spectrumnews.org/
Mayo Clinic Staff Writer (2020). Autism Spectrum Disorder, Overview: Mayo Clinic Rochester, MN.; Retrieved online from – https://www.mayoclinic.org/
Nash, M. (2002). The Secrets of Autism; Time magazine article.
Satel, S. (2014). DSM-IV & DSM-V Differences: Ending the Confusion; Retrieved online from – Counselling Connection > Clinical Mental Health > DSM-IV and DSM-V Differences: Ending the Confusion.
Squaresky, M. (2014). A Spot on the Wall; eBook Edition.
Staff Writer (2013). Autism; Retrieved online from – http://www.autismepicenter.com/
Whiffen, L. (2009). A Child’s Journey Out of Autism: One Family’s Story of Living in Hope and Finding a Cure; eBook Edition.
UNIT 1 – CHAPTER 1 APPENDIX A – Parent Concerns Informal Checklist (Similar to CDC online checklist)
Child’s Name _________________________
Date of Birth ________ Parent’s Name______________
My Child
< Answer (Pick one) Yes, Some-times, or No >
Responds to name
Says 10 (or more) words
Learns new words, weekly
Repeats new words heard
Repeats a new or familiar word over & over, constantly
Says 50 (or more) words
Puts 2 words together, independently
Gets my attention with words
Rejects something by saying “No”
Asks questions by changing voice to indicate s/he is asking a question
Takes turns in a conversation (engages in a back-and-forth)
Asks for help with words
Says understandable 3-4 word sentences
Is easily understood by other family members
Is easily understood by familiar adults
Is easily understood by unfamiliar adults
Follows one-step directions
Follows two-step directions
Listens to story being read in short picture book
Names the pictures in the book (interaction with reader)
Answers “Yes” or “No” questions
Asks “Yes” or “No” questions
Asks “wh” questions (who, when, where, what, why, how)
Uses pronouns correctly (I, me, we… instead of using person’s name)
Knows some songs or nursery rhymes
Participates in pretend play (plays mommy/daddy, teacher, doctor)
Very active, always in motion (hyperactive)
Acts without fear of consequences (impulsive)
Points to objects s/he sees or wants
Unusual reaction to the way things sound, smell, feel, taste or look
Throws tantrums (goal oriented, wants something that’s been denied, needs audience to be watching, trying to get control of others)
Has meltdowns (doesn’t know what’s wrong, it may be ‘sensory’ or other ‘overload’ or s/he may be overwhelmed by what is happening, emotions seem out of control)
Lines up toys or other objects, obsessively, engages in self-stimulatory behavior
Plays with the same toys the same way every time
Needs to follow a routine or ritual (bedtime, eating, and/or getting dressed)
Flaps hands, rocks body, or spins self in circles (or watches spinning things for a long period of time). Add something odd that you are noticing? _________________________
Only eats certain foods
Has difficulty feeding oneself
Can use pincher fingers to pick-up food
Uses utensils to eat food
Seems clumsy or uncoordinated
Can play on age-appropriate playground equipment
Plays well with siblings & same-age children
Note: The above is 'Informal data' to share with clinicians. Video on cell phone is helpful, too.
CHAPTER 1 – RED FLAGS
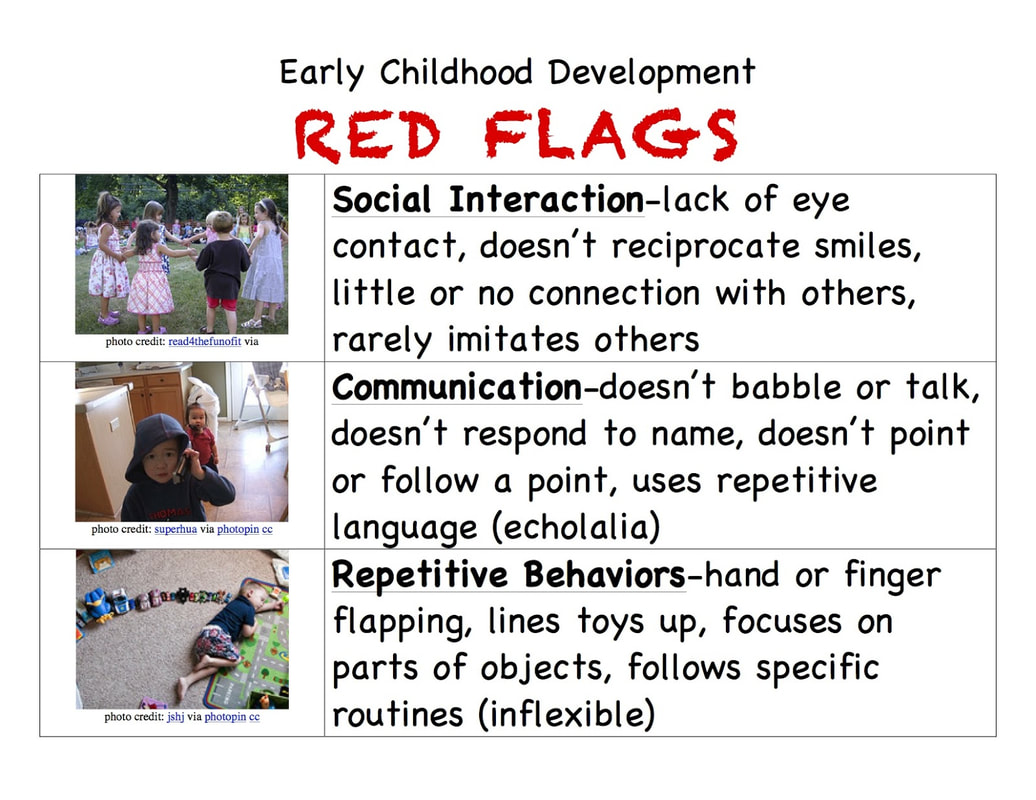
Image shows 'Red Flags', symbols of core symptoms of Autism to be aware of.
Squaresky (2014) insisted that her son Greg looked so normal when he was little. But that people started to stare at him as he became older. It wasn’t so cute anymore to see 2-year-old Greg have a conniption in a store.
Many of the autistic behaviors we see in children with autism are those same behaviors from that of their earlier developmental stage. It’s when your child doesn’t replace those behaviors with a more age appropriate one that it becomes a ‘red flag’ for autism.
Note: In this material, ‘behaviors’ are not addressed separately under a Unit or Chapter titled – ‘BEHAVIORS’, but they are included throughout many of the Units and Chapters. My reasoning is that an individual’s ‘behaviors’ and/or behavior-health concerns are a result of other issues; such as a ‘response’ to what they perceive to be happening in their world, ‘sensory’, ‘communication’, ‘frustration’, issues.
Merchent (2007), a mom who when trying to explain her son Clay’s challenges, exclaims that he’s NOT autistic, ‘but’ –
Those are just the things we know he’s allergic to. Eating is like walking through a minefield.
Luckily, he’s not allergic to wheat, although people keep trying to get us to take him off of it, because so many autistic children are allergic to wheat.
He’s NOT autistic, ‘but’ –
He’s not autistic, ‘but’, I kept hearing myself say as I explained Clay’s behavior, illnesses, and inability to sleep through the night.
Squaresky (2014) insisted that her son Greg looked so normal when he was little. But that people started to stare at him as he became older. It wasn’t so cute anymore to see 2-year-old Greg have a conniption in a store.
Many of the autistic behaviors we see in children with autism are those same behaviors from that of their earlier developmental stage. It’s when your child doesn’t replace those behaviors with a more age appropriate one that it becomes a ‘red flag’ for autism.
Note: In this material, ‘behaviors’ are not addressed separately under a Unit or Chapter titled – ‘BEHAVIORS’, but they are included throughout many of the Units and Chapters. My reasoning is that an individual’s ‘behaviors’ and/or behavior-health concerns are a result of other issues; such as a ‘response’ to what they perceive to be happening in their world, ‘sensory’, ‘communication’, ‘frustration’, issues.
Merchent (2007), a mom who when trying to explain her son Clay’s challenges, exclaims that he’s NOT autistic, ‘but’ –
- For no reason, he bangs his head with his hands, or on window ledges, the asphalt, or the floor.
- He frequently walks on his toes, and sometimes spins in circles.
- He’s extremely allergic to milk, corn, soy, eggs, oats, chocolate, feathers, and dust.
Those are just the things we know he’s allergic to. Eating is like walking through a minefield.
Luckily, he’s not allergic to wheat, although people keep trying to get us to take him off of it, because so many autistic children are allergic to wheat.
He’s NOT autistic, ‘but’ –
- He’s two years old and can only say about eight things, mostly ‘no’; ‘bu’ for ball (which he uses to describe almost everything), and ‘du’ for dad.
- He’s sick most of the time and a cold means at least two weeks of hell for the whole family.
- His nose and chest are constantly congested and mucous shoots down to his chest when he sneezes.
- He doesn’t sleep for more than two or three hours at a time, waking frequently and crying.
- He’s mostly unhappy, grunting and crying; smiling is rare.
- He wants to be held all the time and refuses to walk even though he’s capable; Mommy’s back hurts most of the time as a result.
- He insists on climbing up on the bar in the den every night, and paces back and forth, endlessly. He grunts as he does it. It doesn’t actually make him happy, he’s just ‘less unhappy’. Every night feels like a test of endurance.
- He absolutely hates to ride in the car. A fifteen-minute drive puts Mommy in a full sweat, and an hour drive is out of the question.
- We have to cut his hair when he sleeps, because he becomes hysterical and thrashes around at the barber until we’re afraid he’ll get hurt.
- Noises frighten him so much we carry a headset intended for a gun range, in our diaper bag.
- The tags in his clothes bother him to the point we have to surgically remove them from every shirt to make sure no plastic thread or part of the tag is left to rub his skin.
- His shoelaces have to be tied backwards, because he wants them exactly perpendicular to his leg. He becomes explosive if I forget and hurriedly tie them my normal way.
- He has systemic yeast.
- He makes eye contact, although I frequently find him looking ‘through’ me instead of ‘at’ me.
- He likes to watch fans, although not as much as he did when he was a baby.
- He sometimes crawls on his hands and knees and bizarrely drags his head as he moves across the floor.
He’s not autistic, ‘but’, I kept hearing myself say as I explained Clay’s behavior, illnesses, and inability to sleep through the night.
Image shows child sleeping next to his 'lined-up' toys.
< My Thoughts > “He’s not autistic, but...”
But he may have ‘sensory’ issues, not always thought of as an actual part of autism, in the earlier DSM-4. The latest 2013 Diagnostic & Statistical Manual of Mental Disorders, Fifth Edition, (DSM-5) now includes new criteria for diagnosing ‘sensory’ issues, under the autism umbrella.
Your child may only meet a few of the criteria we can already identify as ‘signs’ of autism. There can be ‘variations’ or ‘severity levels’ of these ‘signs’, according to your child’s ‘developmental’, or ‘autism’ trajectory; alas, autism is a spectrum of disorders.
There are other factors which may be present, such as symptoms of – Attention Deficit Hyperactivity Disorder, Obsessive Compulsive Disorder, Oppositional Defiant Disorder; and the list goes on.
Know too, that the child could also have strong personality issues such as, dad’s stubbornness and/or mom’s need for control. Or, he has tantrums because he wants his shoes to look like his brother’s shoes. All of this may play into the – He’s NOT autistic, ‘but’ list.
Note: More about Personality & Temperament in UNIT 3 Chapter 3, & Sensory in UNIT 4.
Wolff, et al. (2019) say that atypical behavior responses to external ‘sensory’ stimuli are a common feature of ASD. Children with autism can have unusual interests in sensory aspects of the environment. For example, they say that a child may exhibit distress in a noisy classroom, but show no reaction to a loud vacuum. Another example would be that the child insensitive to a wide range of visual and auditory stimuli, may show a marked reaction to being lightly touched.
< My Thoughts > “…atypical behavior responses…”
One might ask – An ‘atypical behavior response’, compared to what? The point here is that parents, pediatricians, and teachers may NOT see a ‘sensory response pattern’, because of the different settings in which they occur. Or, the child may not always have the same ‘sensory’ response each time, possibly because his/her sensory tolerance level is different, that day.
Cohen (2011) says that as a parent she learned about autism from the Red Flag ‘NOTs’; including ‘NOT’ pointing or waving by twelve months, neither of which her son Ezra does.
He hasn’t adopted any of the sign language I’ve been diligently trying to teach him, since he was nine months old.
He engages with us as long as what we are doing interests him. He’s affectionate and doesn’t mind loud noises, or sudden changes; rarely objecting if we want to join him in his play or engage in what he’s already doing. He’s a one-year-old, a baby still. It’s so hard to know.
At eighteen months Ezra learns sign language for ‘more’. I have been trying to teach him for the better part of a year. Pushing my fingertips against each other again and again, saying, “More, Ezra. Look at my hands. More, More.”
< My Thoughts > “He’s not autistic, but...”
But he may have ‘sensory’ issues, not always thought of as an actual part of autism, in the earlier DSM-4. The latest 2013 Diagnostic & Statistical Manual of Mental Disorders, Fifth Edition, (DSM-5) now includes new criteria for diagnosing ‘sensory’ issues, under the autism umbrella.
Your child may only meet a few of the criteria we can already identify as ‘signs’ of autism. There can be ‘variations’ or ‘severity levels’ of these ‘signs’, according to your child’s ‘developmental’, or ‘autism’ trajectory; alas, autism is a spectrum of disorders.
There are other factors which may be present, such as symptoms of – Attention Deficit Hyperactivity Disorder, Obsessive Compulsive Disorder, Oppositional Defiant Disorder; and the list goes on.
Know too, that the child could also have strong personality issues such as, dad’s stubbornness and/or mom’s need for control. Or, he has tantrums because he wants his shoes to look like his brother’s shoes. All of this may play into the – He’s NOT autistic, ‘but’ list.
Note: More about Personality & Temperament in UNIT 3 Chapter 3, & Sensory in UNIT 4.
Wolff, et al. (2019) say that atypical behavior responses to external ‘sensory’ stimuli are a common feature of ASD. Children with autism can have unusual interests in sensory aspects of the environment. For example, they say that a child may exhibit distress in a noisy classroom, but show no reaction to a loud vacuum. Another example would be that the child insensitive to a wide range of visual and auditory stimuli, may show a marked reaction to being lightly touched.
< My Thoughts > “…atypical behavior responses…”
One might ask – An ‘atypical behavior response’, compared to what? The point here is that parents, pediatricians, and teachers may NOT see a ‘sensory response pattern’, because of the different settings in which they occur. Or, the child may not always have the same ‘sensory’ response each time, possibly because his/her sensory tolerance level is different, that day.
Cohen (2011) says that as a parent she learned about autism from the Red Flag ‘NOTs’; including ‘NOT’ pointing or waving by twelve months, neither of which her son Ezra does.
He hasn’t adopted any of the sign language I’ve been diligently trying to teach him, since he was nine months old.
He engages with us as long as what we are doing interests him. He’s affectionate and doesn’t mind loud noises, or sudden changes; rarely objecting if we want to join him in his play or engage in what he’s already doing. He’s a one-year-old, a baby still. It’s so hard to know.
At eighteen months Ezra learns sign language for ‘more’. I have been trying to teach him for the better part of a year. Pushing my fingertips against each other again and again, saying, “More, Ezra. Look at my hands. More, More.”
Image shows placing fingertips together, an action which is a 'sign' for 'more'.
I’m handing him one cheese puff at a time, urging him to ask for more. He looks at the bag, leans toward it, says, “Mm mm mm.” Finally, he does it. He presses his chubby dimpled hands together. He watches them as he does. “More!” I yell. “You signed ‘more’,” I hand him the puff and he sticks it in his mouth, unfazed.
< My Thoughts > “…Ezra learns sign language…”
The inability to communicate one’s wants and needs can be extremely frustrating for anyone. Non-verbal, or even verbal babies and children on the spectrum, often resort to tantrumming in order to express their frustration at not being able to communicate. Our Sonny’s frustration, especially as he becomes older, seems to stem from the knowledge that we are asking him to ‘sign’ for something, when we already know what he wants. But we usually give in, trying again on a different day. A ‘sunnier’ day.
Note: More about ‘Signing’ in UNIT 3, Chapter 2.
Centers for Disease Control & Prevention (CDC) Autism RED FLAGS at 18 months –
< My Thoughts > “…inflexible.”
The Red Flag ‘nots’, ‘doesn’ts’, ‘lack ofs’, and ‘inflexibles’ may mean that the child seldom, or never, gets happily excited over the little things, but may react unhappily instead. There’s little or no ‘back and forth’ responses, reciprocal smiles, giggles or joyful pleasure when with others.
Note: LINKS – https://www.cdc.gov/ncbddd/actearly/milestones/index.html & Module 1: Early Warning Signs of Autism | CDC
Stagliano & McCarthy (2010) share – Of our three daughters, Mia was compliant and passive. Gianna was defiant and overactive. It never occurred to us that they could have the same thing? Eventually, Mia and Gianna were both formally diagnosed with autism.
Mia is our most affected child. If you were to meet her, you’d first notice her great beauty. She speaks in short phrases, mostly to make her needs known. “Can. I. Have. Food. Please.” She’s content to play alone. You can usually find her at her computer, or watching Sesame Street, or Blue’s Clues. She had her first seizure when our third daughter, Bella, was just a babe in arms.
I missed the signs in Gianna. Her cheeks were papery and red. Her nose ran constantly. She had surgically implanted ear tubes as a precaution to help her speech. But her speech still did not develop. Her behavior was atrocious. She spent much of her day screaming and running away from me.
Gianna’s autism moments are usually like bolts of lightning. They strike and then disappear, like she does when she wanders away from us.
< My Thoughts > “…Gianna’s autism moments…”
Along with concerns such as, Mia’s staccato speech, and Gianna’s autism moments, parents have been heard to exclaim –
And, one of the most heart wrenching things to hear – “I need to do something, but I don’t know what to do!”
Stagliano & McCarthy affirmed; they dutifully took Mia to the Children’s Hospital of Philadelphia. From there we contacted a local Early Intervention site. When your child qualifies for help, it’s a bittersweet moment. You’re grateful for the help, trust me. But, in my heart I wanted Mia to blow off the doors of the tests, and tell them all ‘goodbye’.
CHAPTER 3 – CENTERS for DISEASE CONTROL & PREVENTION (CDC) ~
Developmental Screening
(CDC) Centers for Disease Control & Prevention (2020) and the Autism & Developmental Disabilities Monitoring Network (ADDMN), estimate that 1 in 54 American children are born with Autism. In the developing countries throughout the world, the reported numbers vary widely.
I’m handing him one cheese puff at a time, urging him to ask for more. He looks at the bag, leans toward it, says, “Mm mm mm.” Finally, he does it. He presses his chubby dimpled hands together. He watches them as he does. “More!” I yell. “You signed ‘more’,” I hand him the puff and he sticks it in his mouth, unfazed.
< My Thoughts > “…Ezra learns sign language…”
The inability to communicate one’s wants and needs can be extremely frustrating for anyone. Non-verbal, or even verbal babies and children on the spectrum, often resort to tantrumming in order to express their frustration at not being able to communicate. Our Sonny’s frustration, especially as he becomes older, seems to stem from the knowledge that we are asking him to ‘sign’ for something, when we already know what he wants. But we usually give in, trying again on a different day. A ‘sunnier’ day.
Note: More about ‘Signing’ in UNIT 3, Chapter 2.
Centers for Disease Control & Prevention (CDC) Autism RED FLAGS at 18 months –
- Social Interaction – Lack of eye contact, doesn’t reciprocate smiles, little or no connection with others, rarely imitates others.
- Communication – Doesn’t babble or talk, doesn’t respond to name, doesn’t point or follow a pointing. Uses repetitive language.
- Repetitive Behaviors – Hand or finger flapping, lines up toys, focuses on parts of objects, follows specific routines (inflexible).
< My Thoughts > “…inflexible.”
The Red Flag ‘nots’, ‘doesn’ts’, ‘lack ofs’, and ‘inflexibles’ may mean that the child seldom, or never, gets happily excited over the little things, but may react unhappily instead. There’s little or no ‘back and forth’ responses, reciprocal smiles, giggles or joyful pleasure when with others.
Note: LINKS – https://www.cdc.gov/ncbddd/actearly/milestones/index.html & Module 1: Early Warning Signs of Autism | CDC
Stagliano & McCarthy (2010) share – Of our three daughters, Mia was compliant and passive. Gianna was defiant and overactive. It never occurred to us that they could have the same thing? Eventually, Mia and Gianna were both formally diagnosed with autism.
Mia is our most affected child. If you were to meet her, you’d first notice her great beauty. She speaks in short phrases, mostly to make her needs known. “Can. I. Have. Food. Please.” She’s content to play alone. You can usually find her at her computer, or watching Sesame Street, or Blue’s Clues. She had her first seizure when our third daughter, Bella, was just a babe in arms.
I missed the signs in Gianna. Her cheeks were papery and red. Her nose ran constantly. She had surgically implanted ear tubes as a precaution to help her speech. But her speech still did not develop. Her behavior was atrocious. She spent much of her day screaming and running away from me.
Gianna’s autism moments are usually like bolts of lightning. They strike and then disappear, like she does when she wanders away from us.
< My Thoughts > “…Gianna’s autism moments…”
Along with concerns such as, Mia’s staccato speech, and Gianna’s autism moments, parents have been heard to exclaim –
- “My ‘real’ child fades in and out.”
- “How do I build a bridge to him/her?”
- “I catch hopeful moments, then they’re gone like quicksilver.”
- “He’s evaporating before my eyes.”
- “She looks right through me.”
And, one of the most heart wrenching things to hear – “I need to do something, but I don’t know what to do!”
Stagliano & McCarthy affirmed; they dutifully took Mia to the Children’s Hospital of Philadelphia. From there we contacted a local Early Intervention site. When your child qualifies for help, it’s a bittersweet moment. You’re grateful for the help, trust me. But, in my heart I wanted Mia to blow off the doors of the tests, and tell them all ‘goodbye’.
CHAPTER 3 – CENTERS for DISEASE CONTROL & PREVENTION (CDC) ~
Developmental Screening
(CDC) Centers for Disease Control & Prevention (2020) and the Autism & Developmental Disabilities Monitoring Network (ADDMN), estimate that 1 in 54 American children are born with Autism. In the developing countries throughout the world, the reported numbers vary widely.
Image shows CDC Website Logo.
The following website helps parents understand their baby's development. Thus, providing a guide to the developmental milestones, which may help in highlighting concerns to identify and discuss with the baby's doctor.
Note: The Developmental Milestone Checklist can be found on the Centers for Disease Control & Prevention (CDC) website under – Learn the Signs. Act Early; on www.cdc.gov/ActEarly. CDC Learn the Signs. Act Early. Found on – https://www.cdc.gov/ncbddd/actearly/milestones/index.html/
The following website helps parents understand their baby's development. Thus, providing a guide to the developmental milestones, which may help in highlighting concerns to identify and discuss with the baby's doctor.
Note: The Developmental Milestone Checklist can be found on the Centers for Disease Control & Prevention (CDC) website under – Learn the Signs. Act Early; on www.cdc.gov/ActEarly. CDC Learn the Signs. Act Early. Found on – https://www.cdc.gov/ncbddd/actearly/milestones/index.html/
Image shows parent with child. Retrieved from – cdc.gov/MilestoneTracker & https://www.cdc.gov/ncbddd/actearly/milestones/index.html
Hine, et al. (2018) have found in their study that ASD identification, particularly in underserved populations, and despite the good intentions of physicians, have been extremely limited. In order to overcome those existing barriers and long wait times of ASD diagnosis, the Primary Care Clinic setting they studied used a Medical Home Model of healthcare. This model included gathering patient data on sleeping feeding, toileting, behavioral problems, and other behavior-health concerns. This was backed-up with additional electronic medical records, followed by same-day-testing diagnosis; and included direct referrals and possible school-based service options.
< My Thoughts > “…Medical Home Model of healthcare…”
The ‘Medical Home Model’ of healthcare and ‘like’ models are used in many general healthcare agencies now, because it provides a more comprehensive coverage of patient data. Added to updating patient data with each visit, there is a complete notation of visits to ‘new’ providers, their data and recommendations. This also makes tracking easier for insurance company coverage and payment. But, it also requires the patient or parent of the patient to obtain a ‘referral’ to the ‘new’ clinician or therapist, to complete the insurance procedural requirements.
Note: More about ‘Insurance’ coverage in UNIT 6.
Miles (2013) believed that his son, Benjamin, delivered by C-section the day after Christmas, was a genuine Christmas gift. The next six months passed exactly as you would imagine, with diapers and bottles, and many sleep-deprived nights. Ben was a normal happy infant and we were a normal happy-but-exhausted family.
Three months later, at nine months old, I began to be concerned about Ben’s development. He was lagging behind on some of the standard metrics. We compared him to the 6-month CDC ‘Missing’ Developmental Milestones Checklist.
(CDC) Staff Writer (2020) offers a Centers for Disease Control and Prevention Missing Developmental Milestones Checklist for a child at 6 months of age –
- Does NOT try to get things that are within reach
- Shows NO affection for caregivers
- Does NOT respond to sounds
- Has difficulty getting things to mouth
- Does NOT make vowel sounds (‘ah’, ‘ch’, ‘oh’)
- Does NOT roll over in either direction
- Does NOT laugh or make squealing sounds
- Seems very stiff, with tight muscles
- Seems very floppy, like a rag doll
The website advised that parents and pediatricians look for ‘signs’ of the child being to ‘slow’ when meeting developmental milestones. Ben was NOT displaying the kind of cognitive and sensory skills that are expected by that age.
< My Thoughts > “…look for ‘signs’...”
Other signs to look for – the CDC and other websites have lists of developmental expectations, by age group. Continue to look for and list descriptions of your child’s developmental concerns to share with his or her primary physician.
Here is another (CDC) Centers for Disease Control and Prevention list of On-target Developmental Milestone expectations for the 9-month-old child –
- May be afraid of strangers
- May be ‘clingy’ with familiar adults
- Has favorite toys he/she plays with
- Understands ‘NO’
- Makes a lot of different sounds
- Uses fingers to point at things
- Picks up things like cereal between thumb & index figure
- Moves items smoothly from one hand to another
- Plays peek-a-boo
- Looks for things that you hide
How your child plays, babbles, and acts are keys to how he or she is developing.
(CDC) Centers for Disease Control and Prevention advises parents about ‘acting early’ to notify the child’s doctor, when concerned about the way your 18-month-old plays, learns, speaks, acts, or moves. Be concerned, if the child –
- Is missing milestones
- Doesn’t point to show things to others
- Can’t walk
- Doesn’t know what familiar things are for
- Doesn’t copy others
- Doesn’t gain new words
- Doesn’t have at least 6 words
- Doesn’t notice or mind when a caregiver leaves or returns
- Loses skills s/he once had
Tell the child’s doctor or doctor’s nurse if you notice any of these signs of possible developmental delay, and ask for a developmental screening.
If you still feel concerned –
1. Ask for a referral to a specialist. (Referrals are needed for Insurance payment.)
2. Call your state/territory’s early intervention program to find out if your child can get services.
End of excerpts from the CDC checklist. Learn more online, at cdc.gov/Find\. Or, go to cdc.gov/Concerned.
Honigfeld, et al. (2012) believe that the Autism Early Detection Developmental Screening Pilot Program they reviewed, provided promising strategies. For instance, at the 18-month well-child exam, a strategy for changing clinical practice behavior to include engaging pediatricians in developmental screening, and referral to a specialist.
< My Thoughts > “…referral to a specialist.”
When 10-year-old Sonny was referred to a Developmental Psychologist, one of the first things that doctor did was to take several colored plastic blocks out of his desk. Trying not to chuckle, I saw my son’s eyes light up. Sonny was truly engaged and filled with anticipation, as he expected to see the doctor begin stacking blocks; as we have done many times, while trying to teach him how to ‘stack’ blocks. A sort of stare-down occurred, as each waited for the other to begin stacking the blocks. Confusion resulted, and soon the doctor moved on to something else. I have learned to pick my battles and not to try to explain my autistic son’s responses to other people’s world of expectations.
Hinds (2014) has said that one of the hardest things to deal with when you find your child has autism, is that you don’t know the rest of the story. You have no clue how things will turn out. This is why Ryan’s story matters.
My son’s story matters because when parents asked me when I knew Ryan would be okay, I said that I didn’t know he would lead a typical life until much later. I didn’t dare to believe he was actually okay until, as an adult, he was hired by a leading aerospace company and did well. Ryan was happy at work. There he was liked and felt appreciated. And at the same time, more importantly, he had a full social life.
Image shows toddler spontaneously stacking blocks
PART 1. Developmental Screening
Staff Writer (2018) The American Academy of Pediatrics (AAP) recommends developmental screening of ALL children for ASD, at the 18-24-month well-child visits; with or without the child seemingly showing symptoms.
They claim that it’s important to know that ‘screening’ your child is NOT the same as ‘diagnosing’ your child. That if your child has a ‘positive’ screen for ASD, referral for a complete ‘assessment and diagnosis’ by a professional is still needed.
On the other hand, if your child DOES NOT test ‘positive’, but you feel s/he still has challenges, insist on further screening. Usually used for a screening tool is what is called the M-CHAT–R/F (Modified Checklist for Autism in Toddlers–Revised with Follow-up), which is NOT considered to be 100% accurate; so, ask for further assessments if you are still concerned after receiving those results.
Staff Writer (2019) says that whether as a test to see if the child has met certain fine motor skill milestones, or for Psychological and Cognitive skill assessment tests, or as a developmental screening, someone may ask your child to ‘stack blocks’.
The expectations are:
Iannaccone (2018) intrigues us with Swiss Developmental psychologist and philosopher, Jean Piaget’s belief that there was a better understanding of a child’s intelligence, by watching them interact with materials. The extent of a child’s sensorimotor stage of development, he said, could be understood by giving a child an opportunity to manipulate random materials; such as ‘stacking blocks’.
< My Thoughts > “…‘stacking blocks’…”
Because ‘stacking blocks’ has become part of autism assessment diagnostics, you may want to experience that with your child. Work with them, allowing many opportunities to learn about stacking blocks, and/or building something.
Damon (2011) decided that stacking blocks, preferably the old-fashioned wooden kind were fun to do. They make a great noise; they’re very durable, and generally inexpensive. They can be stacked, counted, have numbers and colors on the sides. They can be named and counted. The possibilities are endless.
She exclaims also that she found ‘el cheapo’ plastic cups in rainbow colors – I found five cups of each color; I don’t mean the disposable kind, but the more durable kind. We stacked them, we kicked them with our right foot and then our left foot. We placed small objects carefully in each one, we lay on our backs on the floor and balanced them on our noses, we walked with them on our heads. The fun is absolutely limitless.
< My Thoughts > “The fun is absolutely limitless.”
You may try playing the ‘shell’ game with your child –
Now for more fun, let your child manipulate the cups while you track the ball.
Barron (2011), Judy – On his next pass through the room I stopped my son Sean and plopped him down next to me, on the floor. I busily began stacking blocks onto one another, but he had another idea. He grabbed several blocks and put them on the coffee table. Then he knocked them off onto the floor, throwing himself down to watch them fall. Immediately, he repeated the process.
Odd but harmless, I thought. He will soon tire of that. But, he did it again, and again, and again, and again. Each time that he put the blocks on the table and swept them off, he became more and more enraptured.
“No Sean. No more! Come sit here on the floor with Mommy, we’re going to stack the blocks.” He twisted away and grabbed another block, putting it on the tabletop. I took him by the shoulders and moved him away, putting the block back in the pile on the floor. He whined, not looking at me, and reached for another handful of blocks. Running to the table, he plunked them down, then knocked them off.
I told myself: I’m bigger, stronger, older, and more clever. With patience and firmness, I will teach him that there are some things a child can do, and others he cannot. Simple as that!
< My Thoughts > “…‘Simple as that!”
Ahh, but autism is NOT ‘simple’, anything but! Know your child. Know their autism. Stay the course, you’ll be glad you did.
REFERENCES: UNIT 1 – CHAPTER 2 RED FLAGS, CHAPTER 3 Centers for Disease Control & Prevention (CDC); PART 1. Developmental Screening –
Barron, J. (2011). There’s a Boy in Here: Emerging from the Bonds of Autism; eBook Edition.
(CDC) Centers for Disease Control & Prevention (2020). Developmental Milestones at 6-Months; Retrieved online from – https://www.cdc.gov/ncbddd/autism/hcp-dsm.html-6mo.html/
(CDC) Centers for Disease Control & Prevention (2020). Developmental Milestones at 9-Months; Retrieved online from –
https://www.cdc.gov/ncbddd/actearly/milestones/milestones-9mo.html/
(CDC) Centers for Disease Control & Prevention (2020). Developmental Milestones at 18-Months; Retrieved online from –
https://www.cdc.gov/ncbddd/actearly/milestones/milestones-18mo.html/
Cohen, K. (2011). Seeing Ezra: A Mother’s Story of Autism, Unconditional Love, & the Meaning of Normal; eBook Edition.
Damon, L. (2011). Autism by Hand; eBook Edition.
Hinds, M. (2014). I Know You’re in There: Winning Our War Against Autism; eBook Edition.
Hine, J., Herrington, C., et al. (2018). Embedding Autism Spectrum Disorder Diagnosis Within the Medical Home: Decreasing Wait Times Through Streamlined Assessment; Journal of Autism & Developmental Disorders; V48, p2846-2853
Honigfeld, L., Chandhok, L., et al. (2012). Engaging Pediatricians in Developmental Screening: The Effectiveness of Academic Detailing; Journal of Autism & Developmental Disorders; V42:6, p1175-1182.
Iannaccone, A., et al. (2018). Object Use in Children with Autism: Building with Blocks from a Piaget Perspective; Frontiers in Education: Educational Psychology; February Issue.
Merchent, T. (2007). He’s Not Autistic, But – How We Pulled Our Son from the Mouth of the Abyss; eBook Edition.
Miles, R. (2013). 3500: An Autistic Boy’s Ten-Year Romance with Snow White; eBook Edition.
Staff Writer (2018). Block Stacking Test Expectations; Retrieved online from – https://www.adam-mila.com/milestones/fine-motor-skills/stacking/
Staff Writer (2019). Autism Spectrum Disorder; Retrieved online from – https://www.healthychildren.org/English/health-issues/conditions/Autism/
Squaresky, M. (2014). A Spot on the Wall; eBook Edition.
Stagliano, K. & McCarthy, J. (2010). All I Can Handle, and I Am No Mother Teresa: A Life Raising Three Daughters with Autism; eBook Edition.
Wolff, J., Dimian, A., et al. (2019). A longitudinal study of parent-reported sensory responsiveness in toddlers at-risk for autism; Journal of Child Psychology & Psychiatry; V60:3, p314-324.
(BOOK to be continued...)
PART 1. Developmental Screening
Staff Writer (2018) The American Academy of Pediatrics (AAP) recommends developmental screening of ALL children for ASD, at the 18-24-month well-child visits; with or without the child seemingly showing symptoms.
They claim that it’s important to know that ‘screening’ your child is NOT the same as ‘diagnosing’ your child. That if your child has a ‘positive’ screen for ASD, referral for a complete ‘assessment and diagnosis’ by a professional is still needed.
On the other hand, if your child DOES NOT test ‘positive’, but you feel s/he still has challenges, insist on further screening. Usually used for a screening tool is what is called the M-CHAT–R/F (Modified Checklist for Autism in Toddlers–Revised with Follow-up), which is NOT considered to be 100% accurate; so, ask for further assessments if you are still concerned after receiving those results.
Staff Writer (2019) says that whether as a test to see if the child has met certain fine motor skill milestones, or for Psychological and Cognitive skill assessment tests, or as a developmental screening, someone may ask your child to ‘stack blocks’.
The expectations are:
- 12-16 months = stack 2 blocks
- 16 -18 months = stack 3 blocks
- 18-21 months = stack 4 blocks
- 22-24 months = stack 6 blocks
- 25-27 months = place 3 blocks in a row and push like a train
- 28-31 months = stack 6 blocks trying to make something
- 32-36 months = stack 9 blocks without them toppling over
Iannaccone (2018) intrigues us with Swiss Developmental psychologist and philosopher, Jean Piaget’s belief that there was a better understanding of a child’s intelligence, by watching them interact with materials. The extent of a child’s sensorimotor stage of development, he said, could be understood by giving a child an opportunity to manipulate random materials; such as ‘stacking blocks’.
< My Thoughts > “…‘stacking blocks’…”
Because ‘stacking blocks’ has become part of autism assessment diagnostics, you may want to experience that with your child. Work with them, allowing many opportunities to learn about stacking blocks, and/or building something.
Damon (2011) decided that stacking blocks, preferably the old-fashioned wooden kind were fun to do. They make a great noise; they’re very durable, and generally inexpensive. They can be stacked, counted, have numbers and colors on the sides. They can be named and counted. The possibilities are endless.
She exclaims also that she found ‘el cheapo’ plastic cups in rainbow colors – I found five cups of each color; I don’t mean the disposable kind, but the more durable kind. We stacked them, we kicked them with our right foot and then our left foot. We placed small objects carefully in each one, we lay on our backs on the floor and balanced them on our noses, we walked with them on our heads. The fun is absolutely limitless.
< My Thoughts > “The fun is absolutely limitless.”
You may try playing the ‘shell’ game with your child –
- Place three cups upside down on the floor or table.
- Put a small ball underneath one of the cups.
- Move the cups around several times.
- Have your child track which cup has the ball under it.
Now for more fun, let your child manipulate the cups while you track the ball.
Barron (2011), Judy – On his next pass through the room I stopped my son Sean and plopped him down next to me, on the floor. I busily began stacking blocks onto one another, but he had another idea. He grabbed several blocks and put them on the coffee table. Then he knocked them off onto the floor, throwing himself down to watch them fall. Immediately, he repeated the process.
Odd but harmless, I thought. He will soon tire of that. But, he did it again, and again, and again, and again. Each time that he put the blocks on the table and swept them off, he became more and more enraptured.
“No Sean. No more! Come sit here on the floor with Mommy, we’re going to stack the blocks.” He twisted away and grabbed another block, putting it on the tabletop. I took him by the shoulders and moved him away, putting the block back in the pile on the floor. He whined, not looking at me, and reached for another handful of blocks. Running to the table, he plunked them down, then knocked them off.
I told myself: I’m bigger, stronger, older, and more clever. With patience and firmness, I will teach him that there are some things a child can do, and others he cannot. Simple as that!
< My Thoughts > “…‘Simple as that!”
Ahh, but autism is NOT ‘simple’, anything but! Know your child. Know their autism. Stay the course, you’ll be glad you did.
REFERENCES: UNIT 1 – CHAPTER 2 RED FLAGS, CHAPTER 3 Centers for Disease Control & Prevention (CDC); PART 1. Developmental Screening –
Barron, J. (2011). There’s a Boy in Here: Emerging from the Bonds of Autism; eBook Edition.
(CDC) Centers for Disease Control & Prevention (2020). Developmental Milestones at 6-Months; Retrieved online from – https://www.cdc.gov/ncbddd/autism/hcp-dsm.html-6mo.html/
(CDC) Centers for Disease Control & Prevention (2020). Developmental Milestones at 9-Months; Retrieved online from –
https://www.cdc.gov/ncbddd/actearly/milestones/milestones-9mo.html/
(CDC) Centers for Disease Control & Prevention (2020). Developmental Milestones at 18-Months; Retrieved online from –
https://www.cdc.gov/ncbddd/actearly/milestones/milestones-18mo.html/
Cohen, K. (2011). Seeing Ezra: A Mother’s Story of Autism, Unconditional Love, & the Meaning of Normal; eBook Edition.
Damon, L. (2011). Autism by Hand; eBook Edition.
Hinds, M. (2014). I Know You’re in There: Winning Our War Against Autism; eBook Edition.
Hine, J., Herrington, C., et al. (2018). Embedding Autism Spectrum Disorder Diagnosis Within the Medical Home: Decreasing Wait Times Through Streamlined Assessment; Journal of Autism & Developmental Disorders; V48, p2846-2853
Honigfeld, L., Chandhok, L., et al. (2012). Engaging Pediatricians in Developmental Screening: The Effectiveness of Academic Detailing; Journal of Autism & Developmental Disorders; V42:6, p1175-1182.
Iannaccone, A., et al. (2018). Object Use in Children with Autism: Building with Blocks from a Piaget Perspective; Frontiers in Education: Educational Psychology; February Issue.
Merchent, T. (2007). He’s Not Autistic, But – How We Pulled Our Son from the Mouth of the Abyss; eBook Edition.
Miles, R. (2013). 3500: An Autistic Boy’s Ten-Year Romance with Snow White; eBook Edition.
Staff Writer (2018). Block Stacking Test Expectations; Retrieved online from – https://www.adam-mila.com/milestones/fine-motor-skills/stacking/
Staff Writer (2019). Autism Spectrum Disorder; Retrieved online from – https://www.healthychildren.org/English/health-issues/conditions/Autism/
Squaresky, M. (2014). A Spot on the Wall; eBook Edition.
Stagliano, K. & McCarthy, J. (2010). All I Can Handle, and I Am No Mother Teresa: A Life Raising Three Daughters with Autism; eBook Edition.
Wolff, J., Dimian, A., et al. (2019). A longitudinal study of parent-reported sensory responsiveness in toddlers at-risk for autism; Journal of Child Psychology & Psychiatry; V60:3, p314-324.
(BOOK to be continued...)
DISCLAIMER (2024) Know Autism – Know Your Child: with < My Thoughts > by Sara Luker; 2024
Just to let you know that I, Sara Hayden Luker, have put forth my best efforts in presenting what I have learned about autism, by sharing the stories and studies of those who have gone before us. Any author’s mention of products, services, treatments, and interventions or actions are not to be considered an endorsement, thereof. Know that to some, autism is an ‘unregulated business’. The content of this website material, digital or in any other form does not represent medical advice; nor does it constitute medical suggestions in any way. The material, including any downloadable parts, is for informational and/or educational purposes only. Your download and/or use of any of this material indicates your acceptance of this disclaimer.
This is a Personal Use Electronic Download. By downloading, you hereby agree and acknowledge that you are not acquiring any right, title or interest in, or to, the material; nor any associated copyrights, other than the right to possess, hold and use for personal, non-commercial purposes. Furthermore, you agree that you will: (i) not scan, copy, duplicate, distribute or otherwise reproduce the material(s) to resell, (ii) not use the material(s) for any commercial purposes. By purchasing/downloading you agree to these terms unconditionally. No ‘rights’ are given or transferred.
Just to let you know that I, Sara Hayden Luker, have put forth my best efforts in presenting what I have learned about autism, by sharing the stories and studies of those who have gone before us. Any author’s mention of products, services, treatments, and interventions or actions are not to be considered an endorsement, thereof. Know that to some, autism is an ‘unregulated business’. The content of this website material, digital or in any other form does not represent medical advice; nor does it constitute medical suggestions in any way. The material, including any downloadable parts, is for informational and/or educational purposes only. Your download and/or use of any of this material indicates your acceptance of this disclaimer.
This is a Personal Use Electronic Download. By downloading, you hereby agree and acknowledge that you are not acquiring any right, title or interest in, or to, the material; nor any associated copyrights, other than the right to possess, hold and use for personal, non-commercial purposes. Furthermore, you agree that you will: (i) not scan, copy, duplicate, distribute or otherwise reproduce the material(s) to resell, (ii) not use the material(s) for any commercial purposes. By purchasing/downloading you agree to these terms unconditionally. No ‘rights’ are given or transferred.