Whippery, A. (2019). Families & Providers, Outpatient Surgery Magazine; p27-34.
“We’ll hold him down so you can start the IV.” said one of the brothers “We’ve been through this before and this is the only way it can work.”
Our facility had no protocols for patients with Autism Spectrum Disorder (ASD). We needed to do better. My colleagues and I trialed – A Special Accommodations Program for Children with Autism. Learning that you must change your ‘preoperative’ environment. Here are the reasons why:
- ASD is the fastest rising disability in North America
- More frequently than ‘neurotypical’ patients, ASD patients need sedation or anesthesia for –
- Non-verbal ASD patient care can be stressful for families & providers alike
- Learn to anesthetize without traumatizing the patient
- Improved procedures can help all patients through generalized procedures
< My Thoughts > “Improved procedures…”
The Centers for Disease Control & Prevention (CDC) tells parents that “It is important to understand that children with Autism Spectrum Disorder (ASD) can get sick or injured just like children without ASD. Regular medical and dental exams should be part of a child’s treatment plan.
Taking a child, or adult-child, with autism for a well-check or dental cleaning may not be done that easily. For one thing, most with ASD have the phenomenal memories of past experiences, sensory triggers and super-sonic hearing.
Procedures may be improved, but there are more complexities involved that meet the eye… because each individual is so different. For instance, the Diagnostic & Statistical Manual of Mental Disorders- 5 lists three levels of support which may be needed for patients with ASD –
- Requiring some support
- Requiring substantial support
- Requiring very substantial support
Sonny, was in an adult body, requiring the anesthesia needed for his body size, but his mental age was 2yrs old… on a good day. Then there was his ability to pull it all together in the presence of an attractive and compassionate blonde. But, if he established rapport with her initially, and then the next time he sees her, her hair and face are covered (especially with colored, cloth, paper, or patterned materials) … all bets are off.
We trialed a “Special Accommodations Program” for children with ASD at our institution.
< My Thoughts > “Learning special accommodations…”
Different trigger mechanisms can cause an intolerance of uncertainty, creating anxiety, and possibly, restrictive/repetitive behavior. These things may be helped by engaging the person’s favorite phrases or sayings from familiar DVDs, songs, or stories.
From Cynthia Lord’s 2003 eBook, Rules for David, “So someday… he’ll-wake-up-a-regular-brother…” Follow the Rules – “Come on, David.” I let go of his sleeve, afraid I’ll rip it. When he was little, I could pull my brother behind me if he didn’t want to do something, but now David’s eight and too strong to be pulled.
“Let’s go to the video store,” David says, not moving one inch. “You’re going to the clinic. But if you do a good job, Dad’ll take you to the video store when he comes home.” The video store is David’s favorite place…
Beside me, David checks his watch. “I’ll pick you up at five o’clock.” “Dad will pick you up at 5 o’clock. That’s the rule.” David leaps down the steps. He might not understand some things, but David loves rules.
But remembering the rules doesn’t help. So I reach over, wipe away his tears knowing this will calm him. “Frog you are looking quite green,” said Frog. “I am not a frog,” David sniffles.
Parents and other caregivers can share other ways to enter into their world in order to gain their trust. Some say that persons with autism are the ‘new normal’ because many have normal IQ, but lack the necessary social and emotional knowledge. They seem to be finding their place in society, especially in the world of technology. Perhaps because there you can make your own rules.
Important also, is to always tell the patient what you are doing, and why you are doing it. Repeat the procedure a different way if, what you’re saying doesn’t seem to resonate. Allow cognitive processing time.
Sometimes you have to find a different way into their world. Squaresky (2014) shares this about her son, age four. Greg sat next to me at the kitchen table. I took out a marker and tried to draw Cookie Monster. Unable to communicate with my son verbally, I decided to try to connect with him through art. Greg showed that he was able to learn, but his learning was mainly visual.
I drew Cookie Monster for a month or so, and being unable to draw anything more complex, I didn’t try other characters.
Greg watched, said, “Go Dabba” and “more.” Speech appeared only in bits. After producing each new sketch with scented markers, Greg smelled the Cookie Monsters.
ASD cases are very challenging, often taking providers out of their comfort zone.
< My Thoughts > “ASD cases are very challenging, often taking providers out of their comfort zone.”
- Preliminary staff is different than those at actual visit… or, staff changes with each visit.
- Parents can play different roles at time of surgery… soother, enforcer.
Then, give time for patient to process the unfamiliar information. Bring along communication devices from home.
- Using ‘character’ voices may help… “I have a laser, and I will use it!” “To Infinity, and beyond!” “I need a hug!”
- Social stories…. Gas mask… practice at home… use pedi-needles…
< My Thoughts > “Having a more willing participant…”
The patient’s Sensory Needs can become very important to understand. Bogdashina (2003) says that there are many things that people with autism often seek to avoid –
- External control
- Disorder
- Chaos
- Noise
- Bright lights
- Touch
- Involuntary involvement
Note: External control for those with autism may appear in ‘sensory defensive’ behaviors the types of sensory defensiveness –
- Tactile Defensiveness – avoids being touched or bumped and feeling crowded. May grab or push in order to control being touched.
- Oral Defensiveness – flavors, textures, or temperatures of things in their mouth. May agree to be the one to place something in their mouth.
- Visual Defensiveness – oversensitive to light. May avoid eye contact and startle when lights change or under certain lights, such a fluorescent lighting.
- Auditory Defensiveness – sensitive to certain frequencies and/or loud noises. May cover ears or emit screeching sounds to block out what they are hearing.
- Olfactory Defensiveness – certain smells can cause agitation. May become nauseous and/or vomit and/or defecate in response to the offending odor.
- Gravitational/Postural Insecurity or Defensiveness – irrational fear of change in position and/or movement. May try to elevate their head and/or place their feet on the ground and try to run.
These are complex issues, because any or all sensory reactions can cause any of the above undesirable behaviors. Keep in mind that sensory excitement can trigger stimming (hand-flapping, head-banging, hair pulling, scratching or biting, or whatever seems to break the circuit). These are reactions, not thoughtful actions.
Borutta (2015), in human bodies the most important rhythms are in our heart and brain. Other organs establish their own rhythms to provide for respiration, locomotion, digestion, and other functions necessary for life to continue. A finely tuned system which goes mostly unobserved until illness or trauma temporarily upset that balance.
Traumatic inductions can result in behavior changes, sleep disruption and symptoms resembling post-traumatic stress disorder.
< My Thoughts > “…resembling post-traumatic stress disorder.”
Stress can also be caused by repetitive upsetting thoughts, or flashbacks. Comorbid with autism is often Obsessive Compulsive Disorder (OCD) causing ritualistic behavior which could severely disrupt the surgical process. And, my son cannot tolerate hats, so when it is insisted that he wear a sanitary hat for the surgery, he goes into a compulsive escape behavior.
Then when the friendly staff he’s seen during pre-op, come in with their surgical garb on, he will try to pull everything off of everyone; starting with the hats, surgical gloves, and even their shoe covers. And, if you want Sonny to put his head down then there must be a pillow and directions. "Sonny, put your head on the pillow, please."
Individualized Plans – a pre-op nurse interviews the family, using a pre-op checklist screening form. Through this form, the family shares the patient’s behavior triggers, sensory needs, and how s/he tolerates strangers, according to previous experiences.
< My Thoughts > “…Individualized Plans…to accommodate behavior triggers…”
Be clear about what normal daily meds need to be given and when. Sent mask home to practice… smell may be a problem for those with sensory issues. Perfume… hair covered… color and/or feel of the gowns…
Have staff and family stay to observe any complications from anesthesia, previous aspiration pneumonia. Post-op diet and medication. Have needed things ahead of time, for instance… clear liquids (what does the person like/dislike?), straw (may want one with a minimum volume), what is needed if person vomits, on the ride home. Water analgesic for pain, before anesthesia wears off.
Nonpharmaceutical intervention provides better outcomes.
< My Thoughts > “…Nonpharmaceutical intervention provides better outcomes.”
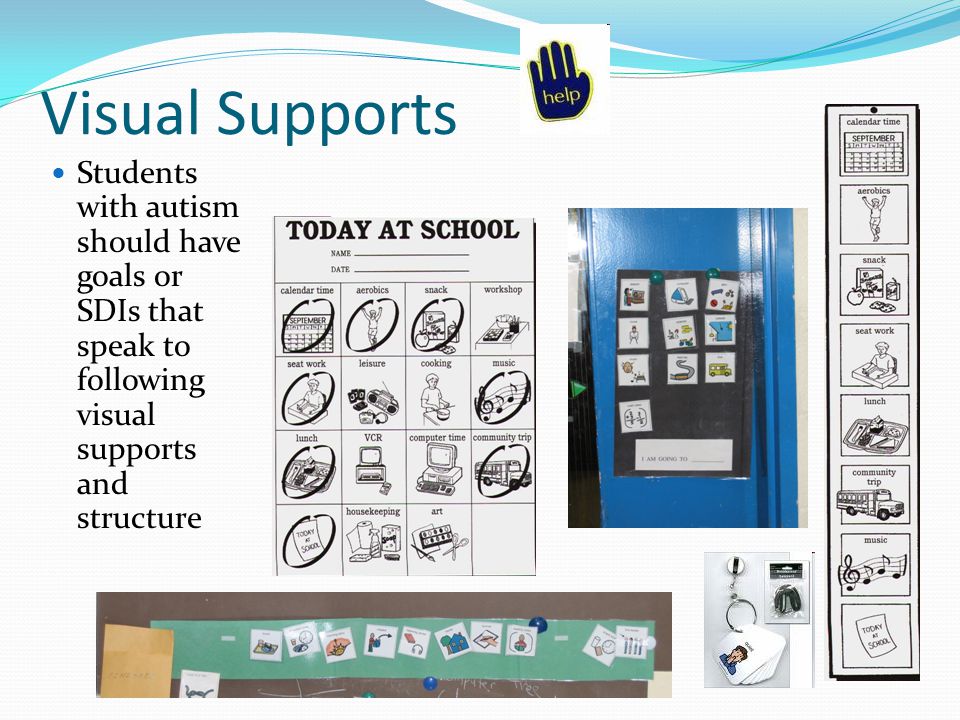
Other ‘nonpharmaceutical interventions which come to mind which may provide a better outcome for patients might be using ‘visual schedules’ and/or ‘social stories’. Another consideration could be to provide a staff member to act as ‘coach’ for staff, patients, and family alike. Much like a ‘life coach’ who guides the process from beginning to end. The protocol for this would be ‘individual’, according to the patient circumstances.
We do everything in our power to minimize stress to our patient to engender cooperation, and to make the patient a more willing participant.
< My Thoughts > “…a more willing participant.”
Make the patient a more willing participant by letting parents be present to a certain point… much like a neuro-typical patient with PTSD. Thomas the Train aficionados may respond to the symbolic phrases – “Stop, the signal is up!” “Apply the brakes, danger ahead!” “Thomas seems sad (frightened, anxious, fearful, etc.).” “Do you know why?” Know also, that most behaviors ignore negative phrases… “Don’t” or “NO!” for instance. Better to tell them the action you desire… “Hands down” or “Wait, please” or “Thanks for staying calm.”
We also exposed them to different scents. The smell of sevofluracane can be a trigger. Send home a mask for practice and reevaluate.
< My Thoughts > “…exposed them to different scents.”
Some scents can trigger sensory reactions. Some children with autism may even vomit or become distressed at the smell of perfume, or other odors. So, the smell, even a faint whiff, of things in the surgery theatre, may become an issue. Or, they may find them stimulating and become excitable. Know that these reactions are involuntary on their part.
On the day of surgery, we will reassess based on how well the child adapted. Streamline the pre-op process.
Make ASD patients first case of the day, because coping abilities may decrease later in the day.
< My Thoughts > “…coping skills…
Some participants may be filled with adrenaline and excitement, first thing in the day. You know those people. I call them the “gett’er done” people. Smiles.
Later in the day, that same person may be exhausted, or at least wound-down. And so what are the staff’s coping skills? Which is better for them, earlier or later in the day? The patient will know those staff members that are not up to dealing with this particular situation and/or patient, no matter what time of day. Trust me on this one!
Different patients may metabolize meds differently.
Individualized plans – we ask patients and family members to visit us for a pre-op meeting with a standardized autism checklist to screen for creating a coping plan. Example of what will be needed to provide a customized experience.
< My Thoughts > “Individualized plans…”
Stay to observe any complications from anesthesia, surgery, bleeding and bruising due to patient’s daily meds, to seizure activity. Post-op meetings could cover the things needed to have handy for the ride home. Drinking using a tiny volume straw to help prevent aspiration problems. Clear liquids and solids, such as apple juice and gelatin, or whatever might be recommended.
Also, make certain the parents understand about ‘nothing by mouth’ before surgery. In some cases, an exception may be the person’s seizure or other necessary medication. And, remember that everyone metabolizes medication differently. Our son had seizures after surgery, if he didn’t have his seizure meds before surgery.
Parents may share that the child may or may not tolerate strangers and healthcare professionals in their space. This includes any physical touching, use of a facial mask, and any IV procedures.
< My Thoughts > “…may or may not tolerate strangers and healthcare professionals in their space…”
Children and adults with autism, when under stress, may see auras. They may also think that ‘everyone else’ in the room sees auras, too. In fact, Zaraska (2016), tells us that the presence of synesthesia is 31% higher in those person’s on the autism spectrum. She goes on to say that scientists believe synesthesia is caused by a hyper-excitability of the visual cortex. Where even the sound of a car honking or a door slamming can trigger seeing colors.
While Lacey, et al. (2016) agree that ‘synesthesetes’ experience an association between seemingly unrelated sensory features.
Remember the staff members who may not be up to dealing with this particular situation? Well, they may be emitting an aura which will influence how things proceed.
For instance – The neuro-typical child may say about someone, “She doesn’t like me!” While the child with autism might say, “When the she comes near me, the soft yellow light around her turns a yucky brown color. Like dirt and things in the toilet.”
Patients appreciate being asked about how to best support their child and stay involved with creating a coping plan. These may include knowing triggers such as loud noises, bright lights, strong smells, strangers, physical touch, transitions, and previous experiences.
< My Thoughts > “…creating a coping plan…”
“Once I give him what I’m going to give him… he’ll be ‘out’… no problems… no seizures.” Wrong!” The child/adult on the spectrum will know this immediately. More extensive coping plans may be needed for some. Make certain that everyone is on board. Some staff members may not be comfortable or flexible with this. Know that –
- What works for one patient may or may not work for the next patient.
- Without their seizure or behavior medications at the usual time and in the regular amount there is a definite risk for an unexpected event.
- Everyone metabolizes medications differently.
- What is the most known fact about autism is that each individual is very different from another.
- The staff member who rehearsed without surgery’s sanitary scrubs, gowns and hats, becomes a whole new person in the eyes of the child/adult with autism.
- Even a new or recent shampoo or body wash or a dangling stethoscope can be problematic.
Some patients find support using a visual schedule with all anticipated steps in the procedure. Other patients may respond to having a coach speaking calmly, guiding and describing each step surgical process. For younger patients, a social story, which they can help design, can show them what to expect.
References used in < My Thoughts > are:
Bogdashina, O. (2003). Sensory Perceptual Issues in Autism & Asperger Syndrome: Different Sensory Experiences – Different Perceptual World; Jessica Kingsley Publishers: London.
Borutta, R. (2019). The Music of the Soul & the Inner Light; Journal for Spiritual & Consciousness Studies, Inc.; V38:2, p113 – 120.
Lacey, S., Martinez, M., McCormick, K., & Sathian, K. (2016). Synesthesia Strengthens Sound-symbolic Cross-modal Correspondences; European Journal of Neuroscience (EJN); V44, p2716-2721.
Lord, C. (2003). Rules for David; eBook 2003 Edition.
Squaresky, M. (2014). A Spot on the Wall; eBook 2014 Edition.
Zaraska, M. (2016). Hear the Violet, Taste the Velvet; Scientific American Mind; V27:6, Nov.
 RSS Feed
RSS Feed